Access Section
The information on this page is intended for health professionals reference and use only. If you are a parent or family member looking for information about treatment, please visit unit information.
Contents
1.0 Aim of guideline
2.0 Scope of guideline
3.0 Guideline summary
4.0 Practice guidelines
4.1 Background information
4.2 Who can care for a PVL?
4.3 Siting a PVL
4.4 Dressing the PVL
4.5 Outgoing care of/maintaining the PVL
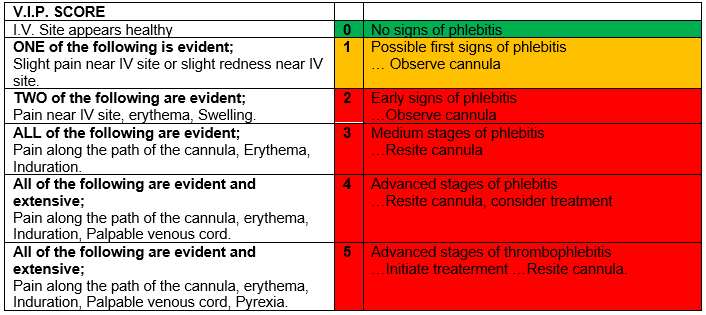
4.6 Fig 1: Visual Infusion Phlebitis score
4.7 Flushing the PVL
4.8 Changing the dressing
4.9 Filters/ Splints/ Protection
4.10 Removal of PVL
4.11 Documentation
4.12 Parents
4.13 Staff education/training
4.14 Resources
4.15 Audit
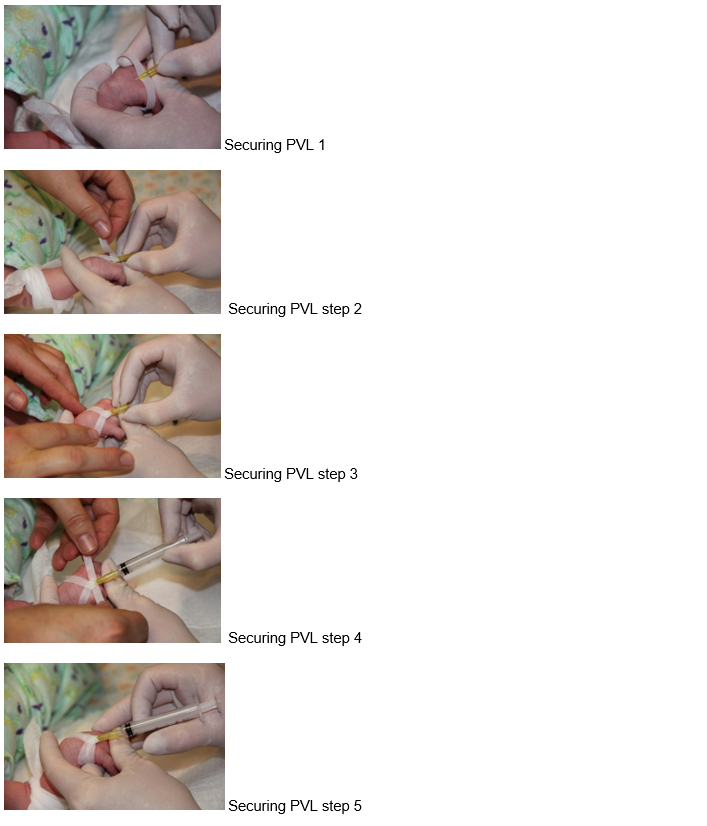
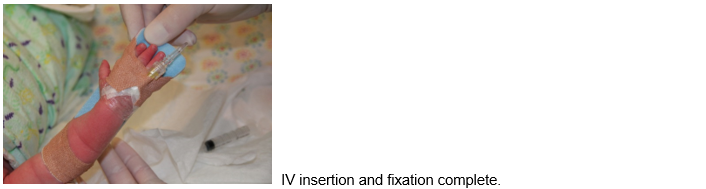
Appendix 1 – Reference photographs for one method of securing a PVL in a neonate
1.0 Aim of Guideline
- To provide a framework to ensure that all infants with a peripheral venous line (PVL) insitu receive the highest standard of evidence-based care.
- Having a PVL insitu puts an infant at risk of infection and therefore requires that all staff caring for the PVL follow evidence-based guidelines. This guideline describes evidence based best practice for care of a peripheral venous cannula.
- Not included within this guideline insertion of a PVL and/ or care of any other type of central, venous or arterial line.
2.0 Scope of Guideline
The guideline applies to all infants with a peripheral venous line (PVL), within Thames Valley and Wessex Neonatal Network Operational Delivery Network.

3.0 Guideline Summary
- All clinical staff may provide care for infants who have one or more PVL in situ.
- Only staff members who have completed their IV administration training and practice assessment, are able to provide full care of a PVL, including regular flushing with saline to assess and maintain the patency of each PVL.
- The aim of caring for a baby with a PVL should be to maintain the patency of the cannula for as long as there is a clinical need. For adults, many hospitals have a policy of routinely replacing a PVL after 72 hours, to minimize the rates of complications. However, on neonatal units PVLs are usually replaced only when clinically indicated.
- The PVL dressing should always be sterile, clear, semi-permeable and polyurethane.
- When the dressing is applied, the baby’s fingers and toes should remain visible, ideally without their range of movement being restricted.
- Use an appropriately sized splint, if necessary.
- When accessing the PVL, aseptic Non Touch Technique should always be used.
- It will sometimes be necessary to change the dressing on a PVL, because it becomes soiled, or has become ineffective at securing the PVL and keeping the site clean.
- It is best practice to regularly assess each PVL using a Visual Infusion Phlebitis (VIP) score. The VIP score is based around a traffic light design, and has been found to improve the process of checking the PVL site. If the score is ‘0’ then the PVL is safe to use. If the score is one, the PVL may be used with caution, and careful monitoring. If the score is 2 or above the PVL must be removed, and appropriate action taken.
- If there is a continuous infusion of fluid or medication running via a cannula every hour staff must assess VIP score and carry out and document a range of observations.
- If the PVL is being accessed intermittently, then at least every 6-12 hours (according to local policy) staff caring for each PVL must assess the VIP score and carry out and document a range of observations.
- If the PVL is being accessed regularly (at least 8-12 hourly) for administration of medicines or fluid then no further flushing will be required. However, where the PVL is being accessed infrequently, the PVL should be flushed at least 12 hourly to assess and maintain its patency.
- Removal of a PVL should be carried out when it is clear that intravenous access is no longer required.
- A PVL will also need to be removed if it is not working effectively, the VIP score is 2 or higher or there is evidence of infiltration and/ or extravasation.
- Staff should provide parents with information about their baby and its PVL, according to their individual needs and preferences.
4.0 Practice Guidelines
4.1 Background Information
Intravenous catheterisation is the most common invasive procedure performed on patients admitted to hospital, as peripheral cannulation provides access for the purpose of hydration, feeding, administration of medications and blood products. However, the procedure exposes the patient to a number of risks, including phlebitis of the vein and infection of the blood stream.
Phlebitis can be mechanical, chemical, infusion or infective in nature, and is the inflammation of the inner lining of the vein, the tunica intima. Clinical signs include localised redness, heat and swelling, which may track further along the vein over time. The patient will feel pain or discomfort, either continuously, or during infusion of drugs or fluids. Catheter related bloodstream infections are caused by similar means as infective phlebitis- where micro-organisms enter the vein through the puncture site. However in bloodstream infections the organisms enter the systemic circulation and can precipitate a blood stream infection.
Many interventions have been developed to reduce the risk of phlebitis including new catheter materials, utilising correct size of cannula, avoiding giving chemically irritant medication via PVL wherever possible, innovative methods for securing, specially designed scoring systems for monitoring PVL status, best hygiene practice during insertion and care bundles for clustering best practice in care of PVL.
4.2 Who can care for a PVL?
- All clinical staff may provide care for infants who have one or more PVL insitu.
- Only staff who have completed their IV administration training, are able to provide full care of a PVL, including regular flushing with saline to assess and maintain the patency of each PVL.
- Staff who will be using the PVL to administer fluids or medications must have undergone intravenous administration training. The training required within each hospital will vary slightly according to local policy, but always includes both practical and theoretical elements, including supervised practice and formal assessment and documentation of competence. All these aspects must be completed before a staff member is considered competent to use and provide full care for a PVL, independently.
4.3 Siting a PVL
This guideline does not include instruction on how to insert a PVL, however, staff caring for a baby with or needing a PVL will often be involved with assisting the health care professional who is siting a PVL, so should be aware of the guidance below;
- If parents are present, explain that the infant needs a PVL and why.
- Parents should be given the opportunity to stay with their baby, whilst the PVL is being sited, particularly if they would like to offer the baby support and comfort during and after the procedure.
- Ensure that wherever possible a new PVL is not sited in a limb that is bruised or has poor perfusion, has had a recent extravasation episode, already has another PVL or peripheral arterial line in situ or is known to be fractured or injured.
- Where possible larger veins should be avoided for siting PVLs (ie greater saphenous vein in the ankles and veins in the ante-cubital fossa) .This is because these are suitable for siting central lines and whenever possible, their integrity should be maintained for this purpose, if required.
- Where possible, veins crossing joints should be avoided for siting PVLs. This is because the baby will naturally flex their ankle, or bend their elbow meaning fluid infusions may not run easily. In addition, the dressing of the PVL can restrict the baby’s limb movement and hence their ability to be positioned comfortably.
- Consider the use topical anaesthetic, if the baby fits the criteria for use (Amethocaine topical from one month post term / Lidocaine with Prilocaine from 37/40 gestation). This needs to be applied over two suitable veins, and held in place with a sterile polyurethane dressing. This needs to be left in situ for the recommended time and then removed before the PVL is sited.
- The baby should be supported through the procedure by someone other than the person siting the PVL, to minimise discomfort and facilitate their coping. This may include some or all of
- Positioning the baby in a midline flexed position, to aid self-comforting and state regulation.
- Swaddling a baby, exposing only the limb the PVL will be sited in.
- Giving the baby a finger or soft piece of fabric to hold.
- Giving oral sucrose or maternal breast milk, just prior to the procedure.
- Non-nutritive sucking during the procedure, using a pacifier, gloved finger or empty breast.
- The person supporting the baby during the procedure may also be required to hold the baby’s limb and assist with the securing of the device.
- If it is necessary to site a cannula in a baby’s scalp, and some of their hair is shaved, ensure that the hair is retained to be given to parents.
- If it is necessary to site a cannula in a baby’s scalp ensure parents are informed of the location of the PVL before they next visit, as some parents will be distressed about their baby’s appearance. They may also need an explanation that the cannula is sited in the vein on the surface of the scalp and is not sited into the brain.
- Sometimes it will be particularly difficult to site a PVL, and multiple attempts may be required to site one. Staff supporting the baby during this procedure need to act as an advocate for the baby, and may need to intervene, and discuss;
- Suggest other staff who may be able to help, ie senior colleagues, anaesthetists
- Equipment/ products that may help- eg different types of cannula, or use of cold light source.
- The ability of the baby to tolerate further attempts.
- Alternative therapies not requiring venous access.
- Alternative methods of venous access, ie long line.
- The need for the baby to have a break before continuing the attempts to site a PVL.
4.4 Dressing the PVL
- The dressing should always be
- sterile
- clear
- semi-permeable
- polyurethane
- Many dressings designed for securing PVLs, come with adhesive strips intended to be sited prior to the clear dressing, to provide extra security. If these are not available, sterile wound closure strips such as Steri-Strips, can be used for this purpose.
- A range of different and equally suitable dressings are available to secure a PVL. If you are not familiar with how to use a particular dressing follow the manufacturer’s instructions and gain help and support from colleagues who have previously used it.
- When the dressing is applied, the baby’s fingers and toes should remain visible, ideally without their range of movement being restricted.
- The PVL should not be covered with bandage, as this prevents visibility of the insertion site, and encourages the retention of moisture
- Use an appropriately sized splint if necessary. The splint can help protect the PVL if the baby is very active. The splint can also help to keep the joint straight, when a baby has continuous fluid infusion through a PVL, allowing an uninterrupted flow of fluid through the PVL.
4.5 Ongoing care of /maintaining the PVL
- The aim of the person caring for a baby with a PVL should be to maintain the patency of the PVL for as long as possible. For adults, many hospitals have a policy of routinely replacing a PVL after 72 hours, to minimize the rates of complications. However, on neonatal units PVLs are usually replaced only when clinically indicated
- If there is a continuous infusion of fluid or medication running via a PVL every hour staff must;
- Visually inspect the site for signs of infusion phlebitis.
- Use the locally agreed Visual Infusion Phlebitis (VIP) score (see the example in Fig 1, below) to score and document any phlebitis seen. This is usually documented on the fluid infusion chart, and must be separately documented for every PVL that is in use and for the duration of any infusions. If any action is required this must be documented too.
- Inspect the dressing, to ensure it is clean and intact. If the PVL dressing is damp or loose, it must be replaced
- If the PVL is being used intermittently, then at least every 6-12 hours (according to local policy) staff caring for it must;
- Inspect the site for signs of infusion phlebitis
- Use the locally agreed VIP score to score and document any phlebitis seen. This is usually on an invasive device record sheet, or a special VIP sticker, placed in the baby’s drug chart If any action is required this must be documented too.
- Inspect the dressing, to ensure it is clean and intact. If the PVL dressing is damp or loose, it must be replaced
- Flush the PVL using saline
- The VIP score is based around a traffic light design, and has been found to improve the process of checking the PVL site. If the score is ‘0’ then the PVL is safe to use. If the score is one, the PVL may be used with caution, and careful monitoring. If the score is 2 or above the PVL must be removed, and appropriate action taken.
4.6 Fig 1: Visual Infusion Phlebitis score (adapted from Jackson, 1998)
4.7 Flushing the PVL
- If the PVL is being accessed regularly (at least 8-12 hourly) for administration of medicines or fluid then no further flushing will be required. However, where the PVL is being access infrequently, the PVL should be flushed at least 12 hourly to assess and maintain its patency.
- The procedure for flushing is outlined below;
- Collect the equipment required on a tray, cleaned according to local policy
- Alcohol wipe x1
- 5 ml syringe (or as dictated by local policy)
- Vial of 0.9% sodium Chloride
- Blunt fill needle
- Gloves
- Clean hands and put on gloves (use apron if required by local policy)
- Draw up the saline flush using Aseptic Non Touch Technique (ANTT), which will be used throughout the procedure. Then dispose of the needle.
- Move to the baby and expose the PVL, to be flushed.
- Remove gloves, apply alcohol gel to hands and apply new gloves.
- Inspect the entry site using locally adopted Visual Infusion Phlebitis (VIP) score.
- Clean the hub / port using cleaning wipe, according to local policy.
- Allow the port to dry naturally
- Attach the syringe to the hub and unclamp the t-extension.
- Slowly flush the PVL, with 0.5-2mls of 0.9% sodium chloride, depending on the size of the baby, the size of the cannula and the ease with which it flushes.
- Clamp the extension whilst still flushing to create a positive pressure
- Observe the site whilst flushing, for;
- Pain
- Swelling
- Leaking of fluid
- Phlebitis
- Extravasation
- Blanching
- If resistance is felt whilst flushing consider;
- Repositioning the limb, especially straightening joints where a PVL crosses them.
- Asking a colleague to try flushing, and give their opinion.
- Replacing the t-extension if it appears to be clogged with back flowed blood.
- Redressing the cannula, as the line may be kinked under the dressing.
- Excessive force should not be used.
- If it is not possible to flush the cannula, despite using these techniques, then it should be removed, according to the guideline below. If there is a continued need for a PVL then a new one will need to be sited, although this may not be immediately necessary.
- Record the VIP score for the PVL and any action taken, clearly documenting which PVL is being referred to, if more than one is in situ.
4.8 Changing the dressing
- It will sometimes be necessary to change the dressing on a PVL, because it becomes soiled, or has become ineffective at securing the PVL and keeping the site clean.
- It is useful to be able to change the dressing, without removing the PVL, and thereby preventing the infant from the trauma and discomfort of having a new one sited.
- Usually two health professionals will be required to carry out this procedure, although a parent may be present if they wish to comfort or reassure the baby.
- Gather required equipment;
- Wash your hands and put on gloves.
- Position baby so that the PVL is exposed and accessible.
- One staff member will often hold the PVL in place, whilst the other carefully removes the dressing.
- Adhesive removal products can be used to assist with the removal process, and minimise damage to the skin. Some dressings have a particular technique for their removal, which is outlined by the manufacturers, ensure you follow these directions.
- Inspect the site of entry for any signs of infection, and if necessary clean the area using sterile gauze and normal saline- or locally agreed skin cleaning product.
- Dry the area if necessary with sterile gauze, then apply a new sterile dressing.
- Return the baby to a comfortable position.
- Dispose of soiled dressing and items used in clinical waste bin.
- Wash your hands.
- Document actions taken.
4.9 Filters/ Splints/ Protection
- When IV infusions and medications are manufactured, there is the possibility that some particulate matter will be present within the fluid. This can be in the form of chemicals, micro-particles, micro bacterial contamination or air. To counteract this risk, many hospitals will use in line filters, when administering any intravenous fluids or medications.
- If local policy requires that a filter is attached to a PVL, the filter must be changed according to local policy. This is usually between every 24 to 96 hours. The filters effectiveness and hygiene status will be diminishing after this time.
- A system must be in place to ensure that all staff know when a filter is first used, so that it is always replaced before its expiry time. This is often recorded on an intravenous device record sheet, or the physical filter is labelled by applying a sticker with the date and time of first use, to the outside of the filter.
- A splint is a product that provides some stability for the PVL, usually by restricting the movement of the limb or joint on which the PVL is sited. If there is a continuous infusion running via the PVL, the splint may help to prevent the joint being flexed, and reduce the chance of occlusion of the infusion.
- The splint also provides protection for the PVL, which can be beneficial if the baby is very active or is dressed.
- If a splint is used, care should be taken to ensure;
- The splint used is designed for the purpose.
- The correct size splint is selected, that effectively supports and protects the PVL, but is not so large that it impedes the baby’s movements or prevents them lying comfortably.
- The limb is splinted in a neutral position
- All fingers and toes are visible and inspected at least every 3-4 hours.
- All fingers and toes are in their natural position, and not bent under or twisted.
- The splint must is not trimmed to size- as many are manufactured with a thin sheet of flexible metal in the middle. Cutting the splint will expose the baby to a very sharp metal edge.
- Ideally, the PVL will not be covered with anything other than the medical dressing. However for a vigorous baby some protection may be required to stop them kicking out the PVL, or sucking on the hub of the PVL.
- The first step would be to ensure the PVL is securely dressed. This can be achieved by using two dressings, placed around the PVL from each end. Additional adhesive strips or steri-strips may also be applied over the vulnerable hub area.
- If this is not sufficient, then it may necessary to cover the PVL with a clean scratch mitt or sock, made out of breathable fabric. The sleeve or foot of a Babygro can also pulled out, to cover the PVL. This technique is also useful if the baby has been scratching their face or skin with the PVL.
- If the PVL is covered, any covering must always be removed before using the PVL, and to enable full and regular inspection.
4.10 Removal of PVL
- Removal of a PVL should be carried out when it is clear that intravenous access is no longer required, if there is any doubt about this, then staff should consult with senior colleagues or other members of the MDT.
- A PVL will also need to be removed if it is not working effectively, the VIP score is 2 or higher or there is evidence of infiltration and/ or extravasation.
- Gather equipment required
- Wash hands
- Put on gloves
- Carefully remove the old dressing whilst leaving the PVL in place.
- Adhesive removal products can be used to assist with the removal process, and minimise damage to the skin. Some dressings have a particular technique for their removal, which is outlined by the manufacturers, ensure you follow these directions.
- Hold the sterile gauze against the entry site
- Slowly remove the cannula maintaining a neutral angle.
- Apply gentle pressure to the exit site, over the top of the gauze.
- Examine the removed PVL and ensure it is intact.
- Inspect the site to ensure bleeding has stopped, but do not wipe the exit site as it may dislodge the thrombus and reactivate bleeding.
- Apply a sterile plaster (according to local practice).
- Dispose of soiled dressing and items used in clinical waste bin.
- Wash your hands.
- Document actions taken.
4.11 Documentation
- Documentation required will vary slightly between neonatal units, depending on their local policy, however it would be usual to document;
- the insertion date, time and location
- the make, product and catheter size used.
- name of the practitioner inserting the device.
- the number and location of unsuccessful attempts- if applicable.
- the VIP score every hour, for a PVL with a continuous fluid infusion.
- the VIP score each time the PVL is used to administer medications or fluid boluses.
- the VIP score at least 12 hourly if a PVL is not in active or regular use.
- if the VIP score is 1 or higher the concern/ issue causing this score must be recorded and any action taken.
- the date and time a PVL is removed.
4.12 Parents
- Staff should provide parents with information about their baby and its PVL, according to their individual needs and preferences. Information they are likely to want to know includes;
- The general purpose of a PVL
- If a new PVL is sited, or needs to be sited, and why.
- If a PVL is removed.
- Any complications experienced by their baby which relate to the PVL.
4.13 Staff education/ training
- The MDT staff should receive training in the care of PVLs during their orientation.
- The TV&W Preceptorship/Foundation Programme provides an IV module that covers training to acquire the theoretical knowledge. Once that is completed, the educators in each unit will provide the practical skills training. A certificate of completion is provided following completion of both elements.
- Staff should provide care for a PVL based on their level of competence and training.
- Usually nursery nurses and staff nurses who have not completed IV assessment can care for a baby who has a PVL in situ. However they will need to ask a colleague to flush the PVL and assess the VIP score, also to administer IV medications, if required.
- Only those staff who have completed and passed their IV assessment may flush a PVL with saline, or administer any fluids or medications through a PVL.
4.14 Resources
- Resources should be available to enable best practice in care of PVLs. This should include;
- Range of suitable cannula types and sizes.
- Supply of sterile dressings suitable for neonates.
- Splints in a range of sizes.
- Supply of VIP score stickers/ infusion device record sheets.
4.15 Audit
- Audit is an important part of monitoring best practice, which aims to help raise standards and promote best practice.
- All staff should be willing to participate with audit that is occurring on the unit relevant to PVL use and care. This is most likely to take the form of benchmarking practice or auditing compliance with PVL policy, auditing rates of complications such as episodes of extravasation, phlebitis or blood stream infection.
Appendix 1 – Reference photographs for one method of securing a PVL in a neonate
See reference photographs for one method of securing a PVL in a neonate. Images take from Safer Care Victoria (2018).

Version control
| Version | Date | Details | Author(s) | Comments |
| Version 1 | July 2017 | Reviewed- awaiting ratification | KR (Chair) | |
| Version 2 | Dec 2019 | Ratified by Governance | ||
| Version 3 | Nov 2023 | For ratification in Nov 23 Governance – ratified | KR (Chair) | CH, SH & RT comments incorporated |
| Review Date: | November 2026 | |||
Document version
Version 3
Lead Authors
Thames Valley & Wessex Neonatal ODN Guidelines Group
Approved by
Thames Valley & Wessex Neonatal ODN Governance Group
Approved on
23 November 2023
Renew date
November 2026
Full guide
Related documents
Ainsworth.S and McGuire.W (2015) Percutaneous central venous catheters versus peripheral cannulae for delivery of parenteral nutrition in neonates (Review) Cochrane database of Systenatic Reviews, Issues 10, Art No CD004219 www.cochranelibrary.com
Ayton-Smith.G and Lawson.T (2014) PVC care policy, Neonatal Unit, St Peter’s Hospital, p 1-4. Found at http://www.asph.mobi/Guidelines_Neonatal/Cannulation%20Care%20Policy.pdf
BNF (2016) BNF for children. Sept 2015-16. BNF.org, BMJ group, RCPCH Pulishing.
Dougherty. L and Lister. S (2020) Royal Marsden Hospital Manual of Clinical Nursing Procedures, (Professional edition)10th Edition, Wiley.
Evans. C and Dixon. A (2006) Intravenous therapy: Practice Issues. Infant, Vol2, Issues 4, pp133-39.
Gallant P and Schultz AA (2006) Evaluation of a visual infusion phlebitis scale for determining appropriate discontinuation of peripheral intravenous catheters. Journal of Infusion Nursing. vol. 29, no. 6, p. 338-45.
Hallam C, and Denton A (2020) Vessel health and preservation 1: minimising the risks of vascular access. Nursing Times [online]; Vol 116: no 7, pp 22-25. Found at www.nursingtimes.net
Hallam C, and Denton A (2020) Vessel health and preservation 2: inserting a peripheral intravenous cannula. Nursing Times [online]; Vol 16: No 8, pp38-41. Found at www.nursingtimes.net
Finch. G and Smith. A (2019) Peripheral Venous catheter insertion and care (NICU) V4, Ashford and St Peter’s Hospital, NHS Foundation trust. Found at ; https://ashfordstpeters.net/Guidelines_Neonatal/PVC%20Guideline%20Mar%202020.pdf
Jackson. A (1998) Consultant Nurse, Intravenous Therapy & Care, The Rotherham NHS Foundation Trust. Original article Jackson A. (1998) A battle in vein: infusion phlebitis. Nursing Times. 94 (4), p.68-71
Marsh.N et al ( 2017) Devices and dressings to secure peripheral venous catheters: A Cochrane systematic review and meta-analysis. International Journal of Nursing Studies, Vol 67, Feb, pp12-19.
RCHM (2014) Peripheral Intravenous (IV) Device management. P1-8, Found at www.rch.org.au/rchcpg/hospital_clinical_guideline_index
Safer Care Victoria (2018) Peripheral Intravenous (IV) catheter insertion for neonates. Women and Children, Safer Care Victoria. Found at; https://www.safercare.vic.gov.au/clinical-guidance/neonatal/peripheral-intravenous-iv-catheter-insertion-for-neonates
Thigpen.J (2007) Peripheral Intravenous Extravsation: Nursing procedure for Initial Treatment. Neonatal Network, No 6, Nov/Dec . pp379-84.
Webster J et al (2019) Clinically‐indicated replacement versus routine replacement of peripheral venous catheters. Cochrane Database of Systematic Reviews 2019, Issue 1. Art. No.: CD007798. DOI: 10.1002/14651858.CD007798.pub5. Accessed 07 June 2023.
Implications of race, equality & other diversity duties for this document
This guideline must be implemented fairly and without prejudice whether on the grounds of race, gender, sexual orientation or religion.