Respiratory Section
The information on this page is intended for health professionals reference and use only. If you are a parent or family member looking for information about treatment, please visit unit information.
Contents
1.0 Aim of guideline
2.0 Scope of guideline
3.0 Guideline summary
4.0 Guideline framework
4.1 Background information
4.2 Practice guidelines
4.21 Prior to commencing CPAP
4.22 Humidification
4.23 Hats and headgear
4.24 Positioning of the CPAP and the baby
4.25 Tubing
4.26 Nasal prongs
4.27 Masks
4.28 Pressure and flow
4.29 Weaning off CPAP
4.30 General care
4.31 Parents
4.32 Documentation
4.33 Care of the nose and face
1.0 Aim of guideline
To provide a framework to ensure that all infants receiving CPAP/ BiPhasic CPAP are optimally cared for.
2.0 Scope of guideline
The guideline applies to all babies receiving CPAP/ BiPhasic CPAP within Thames Valley and Wessex Neonatal Operational Delivery Network.

3.0 Guideline summary
- Continuous heart rate, respiratory rate and oxygen saturation monitoring should be in place, with 6hrly blood pressure checks
- Hourly observations should be performed and recorded for each infant. See list under 4.33
- Decision on CPAP pressures and gas flow should be made between the medical and nursing staff and documented in the care plan and notes
- Weaning from CPAP should be according to local written weaning protocol which is based on the baby’s condition. See guidance under 4.29
- Staff should be vigilant for signs of pain and discomfort or distress and should seek to modify baby’s environment and offer developmental care where appropriate
- CPAP circuits should be humidified at all times. Humidification is delivered to the infant at 37°c
- Sterile water is used to fill humidification chambers
- There is a risk that babies’ noses become squashed and pushed upwards or damaged whilst receiving CPAP, correct positioning should be used to prevent this
- Ensure correct size and fit of hat/ headgear- see 4.23 for details
- The area behind a baby’s ears can become moist with dead skin collecting there under the CPAP hat, so should be checked and cleaned at least daily
- Time and care should be taken to ensure that CPAP is secure, well-fitting and safe. See guidance under 4.24 and 4.25
- It is considered best practice to rotate the use of nasal prongs and nasal mask for a baby receiving CPAP. This should be individualised for each baby, but usual practice is interchanging these 4- 6 hourly
- There should be careful monitoring of skin integrity of the nares, as there is a high risk of damage to the external skin and/or internal membranes of the nose. Appropriate risk assessment / skin integrity score should be used- see 4.33
- Due to a risk of air building up in the baby’s stomach, all babies on CPAP should have an oro-or nasogastric tube in situ. The tube should be aspirated a minimum of every four hours to remove air, and more frequently if required
- If the baby is stable parents/carers should be encouraged to have cuddles and skin to skin care with their baby
4.0 Guideline framework
4.1 Background information
Continuous Positive Airway Pressure (CPAP) became a widely accepted means of respiratory support for term and preterm infants after it was first used by Gregory and associates in 1971 to bring about a significant decline in the mortality rates for neonatal respiratory distress syndrome (RDS).
Physiological effects of CPAP in neonates include improved oxygenation, maintenance of lung volume, reduced upper airway resistance, regularisation of respiratory rate and a reduction in obstructive apnoea CPAP has been found to be beneficial in many neonatal contexts and conditions which is a major reason for its use and popularity in current practice. Listed uses include;
- Prevention of extubation failure
- Apnoea of prematurity
- Alternative to intubation and ventilation in RDS
- Extremely preterm neonates
- Infants with chronic lung disease
In practice CPAP consists of a controlled flow of gas, (either air or an air and oxygen mixture) administered to the baby using a ‘flow driver’ to circulate humidified gas through a CPAP circuit to the larynx or nose.
The ‘level’ of CPAP administered to a baby is measured as a pressure reading of cmH2O. In order to raise or lower the pressure given to a baby the flow of gas in l/min can be increased or decreased.
When CPAP was first used it was given via an endotracheal tube, headbox or face chamber. As equipment and techniques have improved CPAP is now usually given by silicone nasal mask or soft moulded nasal prongs held in place by a specially designed hat. This method is often most well tolerated by an infant and allows access to the baby’s head and mouth and easy movement of the baby.
Despite the many documented benefits of CPAP it is a form of respiratory support that has i complications and can be time consuming and tricky to administer effectively. For example, CPAP relies on maintaining constant pressure within the thorax, so the nasal prongs or mask distorting, the baby moving or simply the baby opening its mouth can cause sudden swings and loss of pressure.
Traumatic injuries to the nose are the most common complication of CPAP in neonates. Nasal prongs may rub and damage the internal aspects of the nasal septum whereas nasal masks are found to cause trauma or lacerations at the junction between the nasal septum and nasal philtrum. Both of these problems can be minimised by good nursing techniques. Other complications include a two to three fold increase in the risk of pneumothorax, gaseous distension of the stomach and difficulties identifying when a baby is ‘failing’ on CPAP and requires more intensive intervention
These guidelines have been produced to direct nursing staff in their care of neonates receiving CPAP and are based on research findings and agreed current best practice. For accessibility, the guidelines have been collated under distinct subheadings, in the order that information is likely to be needed in practice. However, the reader is strongly advised to read the guidelines in full and to seek the advice and support of more senior or experienced colleagues in the practice setting.
4.2 Practice guidelines
4.21 Prior to commencing CPAP
- In recent years CPAP is no longer the most commonly applied form of non-invasive respiratory support for preterm or unwell term infants. Instead, nasal High Flow Therapy is used most commonly due to its potential advantages over CPAP. The consequence of this is that CPAP is used in a neonatal unit less often, and when a baby is more unstable. Both these factors increase the risk of less safe and less effective nursing care of the baby. Caution should therefore be taken, by the nurse co-ordinating a shift, to ensure that an appropriately trained nurse is allocated to look after any baby requiring CPAP support.
- Infants should be nursed in a safe environment. There should be access to suction, oxygen and resuscitation equipment at the bedside. These should be checked at the beginning of each shift.
- CPAP drivers, circuits and humidifiers should be clean and well maintained
- The CPAP driver and associated cables and tubing should be used in accordance with health and safety guidelines
- The CPAP stand should have brakes on it and these must be used
- The flow should be set to local guidelines, usually around 8Lpm and oxygen at the infant’s current requirement
- PEEP (positive end expiratory pressure) should be set based on the infant’s current condition and local guidelines, ‘normal’ initial PEEP is 5cm H2O
- Alarms on the CPAP should be set according to the manufacturer’s guidance. Guidance cards showing this should be readily available, along with equipment manual.
4.22 Humidification
- CPAP circuits should be humidified at all times
- Ensure that the humidifier is on and warmed prior to connecting to an infant. Failure to do this may lead to a cold infant
- Sterile water is used to fill humidification chambers
- Don’t overfill the humidification chamber, don’t let it boil dry
- Humidification is delivered to the infant at 37°c
- When the option is available on the humidifier, set to humidify in ventilation mode
4.23 Hats and Headgear
- Refer to manufacturer manuals / website and training videos for correct fitting of hat/ headgear and related CPAP systems.
- There are a variety of types of bonnet, hat and headgear, now used and available to fix the CPAP system in place on the baby. Each CPAP machine, and circuit system will have hats and headgear designed specifically to interface with their own system, so care must be taken to use the correct one for the correct machine, and circuit.
- For each system there will be a variety of sizes of hat/ headgear available. Often, a colour coded ‘tape measure’ or ‘sizing guide’ will come with the products and allow correct selection of the hat or head gear.
- Take care to follow the instructions carefully. For example if asked to ‘measure’ the baby’s head circumference, this may show applying the tape where the hat will lie at the base of the neck to the line of the forehead and NOT the commonly measured frontal-occipital head circumference.
- Sometimes it will be necessary to go up or down a hat/ headgear size to ensure the best fit, and therefore the best result from the CPAP support.
- The hat/ headgear size should be reviewed weekly, or according to local policy, and documented.
- The hat/ headgear should be positioned according to manufacturer’s instructions. But should never infringe on the eyes, or deform the ears in any way.
- If using an open ended bonnet, the open end of the bonnet should be tied off to ensure a snug and secure fit.
- The hat/ headgear is single patient use only and should not be washed and reused.
- The hat should be changed when dirty or elasticity is lost.
4.24 Positioning of the CPAP and the baby
- There is a risk that babies’ noses become squashed and pushed upwards whilst receiving CPAP, particularly using full contact nasal prongs.
- It has been found that correct positioning can prevent nasal damage and discomfort, so every effort should be taken to ensure that CPAP is secure, well-fitting and safe.
- Things that will help include;
- The CPAP driver should be at the foot end of the incubator or cot, as this most readily allows CPAP tubing to be coming away from the baby so that it follows over the top of the head and down the line of the spine.
- Where the CPAP driver cannot be at the foot of the bed space, ensure that the tubing is following the line of the body,
- CPAP should not be pulled tight, just enough to achieve a seal.
- Do not use gauze or dental rolls between the cheek and the CPAP straps
- Consideration must be given to the developmental needs of the baby, and each baby should have individualised assessment and positioning, which considers their respiratory, comfort, developmental and social needs.
- See the Thames Valley Wessex Neonatal ODN Positioning and Handling Guideline for further information.
4.25 Tubing
- Expiratory tubing should always be outside of an incubator, or at the point furthest away from the baby if nursed in a cot
- Silencers or filters may be required- depending on the manufacturer brand of tubing being used. These are fitted at the end of expiratory tubing and do not reduce the noise level for the baby, but act as bacterial filters
- Where required they should be changed according to manufacturer’s guidelines. However, if the silencer becomes filled with condensation before this time limit, it should be changed sooner, as high levels of condensation in the filters will increase the resistance of gas flow through the filter, and cause the baby increased expiratory effort
- CPAP circuits are for single patient use and should be changed as per manufacturer’s guidelines and recommendation
- Water vapour condenses and gathers in the CPAP tubing, this needs to be removed as soon as it is noticed, because it is very noisy for the baby when it swings in the tubing and can also move and blow into the baby’s nose causing distress and affecting breathing
- Some CPAP circuits, such as EME tubing has a number of slits in the expiratory tubing to allow excess pressure to be released without harming the baby. The slits run down the whole length of the expiratory tubing and are NOT an indicator of faulty or damaged tubing
4.26 Nasal prongs
- Use the sizing guide provided by the manufacturer to correctly gauge the size of prongs needed
- Prongs should be positioned correctly, however what is understood as ‘correct positioning’, will vary according to the design and specification of brand of prongs being used. For every product the specific manufacturer’s instructions for application must be used, to ensure comfort for each baby and to prevent damage to the lateral walls of the nostrils and the nasal septum
- It is not acceptable practice to tightly tie or secure tapes in any way to restrict the movement of the prongs
- Prongs should be changed once a week, or sooner if necessary. In order to keep them clean, patent and free from any obstruction
- The use of dressings is NOT recommended as a preventative measure to protect the skin. Correct fitting of the prongs/ careful observation of the nose and immediate response to any indicators of nasal damage should be employed instead. If skin protection is used, ensure that it is secure and that it cannot migrate into the nostrils or airway passages and block them.
- See point 4.33 ‘Care of the nose and face’, for more information
4.27 Masks
- Research has found that CPAP with a mask as the interface, is as effective as nasal prongs but causes less nasal trauma
- It is considered best practice to rotate the use of nasal prongs and nasal mask for a baby receiving CPAP. This is done to vary the areas of high pressure on the internal and external surfaces of the baby’s nares, in the belief that pressure damage to the skin or mucous membranes will be minimised. Individual judgement is required as to how often to disturb the baby and swap between the prongs and mask- but usual practice is between 4-6hourly
- Sometimes it will be necessary to use only the prongs or mask. This is often because there is nasal trauma in a specific area that is avoided by one or other device, or sometimes even the smallest prongs do not fit the extremely low birth weight infant
- Use the sizing guide provided by the manufacturer to correctly gauge the size of mask needed
- Position correctly and securely to minimise gas leak, especially to the eyes. The eyes should be clearly visible without any of the mask touching them
- Take extra care to ensure that the nose is not pulled upwards to minimise trauma to the base of the nasal septum, which is most at risk when using a mask
- Masks should be changed once a week if necessary, in order to keep them clean, patent, and free from any obstruction
- For the majority of babies, skin protection is not needed or necessary, however, babies who are receiving prolonged mask CPAP may benefit from some protection – refer to nasal skin care policy
- Observe for any indentation into the nose and base of septum (this can be cut by the mask and not be visible without careful examination), around the nose and the bridge of the nose
4.28 Pressure and flow
- Pressure varies greatly depending on the infant’s condition. Initial PEEP is usually 4-6cm H2O, however, effective CPAP can vary between 2-10cm H2O
- Pressure is achieved by altering the flow. Usual flow is between 4-14L/pm
- Decision on pressures and flow should be made between the medical and nursing staff and documented in the care plan and notes
- Indications for adjusting pressure are:
- degree of RDS
- effort of breathing
- chest x-ray results
- oxygen requirement
- unsatisfactory blood gas
- apnoea, bradycardia and desaturation events
- Medical staff should be informed of any change in the infant’s condition and a blood gas should be considered.
- If you need to increase the pressure significantly, then inform the medical staff and nurse in charge, as this could be indicative of a more serious problem, i.e. pneumothorax or need for intubation and ventilation.
4.29 Weaning off CPAP
- Weaning from CPAP should be based on the baby’s condition and according to local written weaning protocol. At the current time there is no definitive evidence to identify which is the best way to support a baby until they no longer require CPAP. However, of three commonly used methods, two are currently recommended.
1) ‘Gradual Weaning’ is where the baby stays continually on CPAP, but the PEEP setting is weaned as the baby’s condition indicates it is able to receive less respiratory support. When the CPAP support is at a low level, the CPAP is then removed and support discontinued. Low flow oxygen can then be used if the baby still has an oxygen requirement.
2) ‘Stepdown Strategy’ is where the baby is switched from CPAP to High Flow Nasal Cannula, or low flow nasal cannula and continues to use this ‘lower’ level of respiratory support for as long as needed. Research has shown that babies weaned using this method have a reduced time on CPAP, but a significantly longer on oxygen supplementation. (Van Delft, 2020). - ‘Interval training’ is where the baby is cycled on and off CPAP over a number of days or weeks. A systematic review of CPAP weaning found this method offered no benefit over sudden discontinuation of CPAP and should ‘probably not be applied in preterm infants’. (Van Delft, 2020, page 1).
- Whichever method is selected the same general principles of care apply;
- document planned weaning regime
- document how baby coped with regime
- if a baby is having time off CPAP but still requires oxygen this can be given via low flow cannula, head box or incubator oxygen
- if baby does not manage planned time off, consider a shorter period off next time, or a longer time on CPAP between cycles, to allow the baby more time to recover. (consult with medical team)
- if a baby is off CPAP and has a desaturation or bradycardia, this does not necessarily mean the baby has to go back onto CPAP. The occasional desaturation or bradycardia may be ‘normal’ for See the list below for guidance.
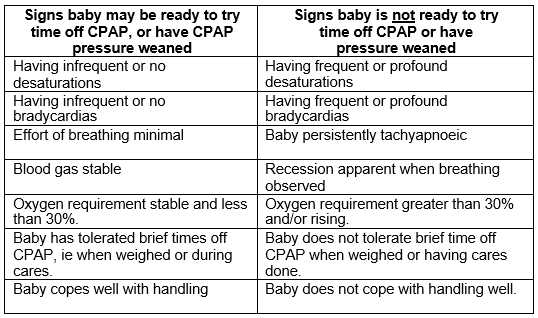
If you are uncertain whether a baby is coping with their regime consult with the medical team or nurse in charge.
4.30 General Care
- Suction may be required, this should be available and individualised to the infants needs
- Continuous heart rate, respiratory rate and oxygen saturation monitoring should be in place. There should be access to a blood gas machine
- Being nursed on CPAP is known to reduce venous return. This does not usually cause clinical complications for a baby, but in order to monitor for any compromise in the baby, every baby on CPAP should have their blood pressure checked at least 6 hourly
- An oro-gastric tube should be used in preference to a naso-gastric tube, to prevent distortion of the nostrils and ensure a good seal of the prongs/mask. This should be aspirated prior to feed to empty gas and reduce the risk of abdominal distension, although CPAP rarely causes a distended abdomen
- If a baby is not being fed, the oro-gastric tube should be aspirated a minimum of every four hours, and more frequently if required. It is possible to leave the tube open or a syringe barrel on the end, but you may get stomach contents passed up through it.
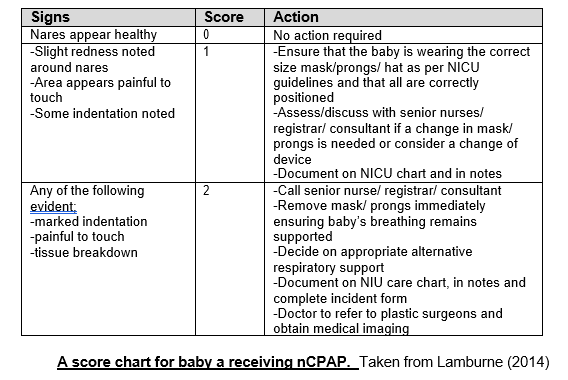
- There should be careful monitoring of skin integrity of the nares, as there is a definite risk of damage to the external skin and/or internal membranes of the nose. Best practice for nose care is for the nose and surrounding area to be assessed and scored on an hourly basis, so that evidence of skin breakdown is identified quickly and managed appropriately. The score should be documented in a predetermined place, the ITU/HDU observation chart would be an appropriate place. See the example below;
- Ensure that the face is kept clean and free from secretions
- Ensure the area behind a baby’s ears is kept clean, as very preterm babies may be nursed with a CPAP hat on 24 hours a day for many weeks in a row
- If transferring a baby on CPAP within a hospital or between hospitals refer to local transportation guidelines and policies
- If there is a significant change in a baby’s support requirement or respiratory status, inform the medical staff and the nurse in charge, as this may be indicative of a more serious problem
- CPAP can be an uncomfortable and unpleasant experience for babies due to the loud noise levels, high gas flow through the mouth and nose, restricted head movements and obstructed faces. Staff should be vigilant for signs of pain and discomfort or distress and should seek to modify baby’s environment and offer developmental care where appropriate. For example, kangaroo care, nesting, non-nutritive sucking, containment holding or a cuddle.
4.31 Parents
- Keep parents/carers informed about their baby’s progress on CPAP.
- Encourage and support parents/carers to interact with and care for their baby whilst on CPAP.
- If the baby is stable parents/carers should be allowed to cuddle and have Kangaroo care with their baby.
4.32 Documentation
- Use local CPAP care plan if available
- One hourly observations should be performed and recorded for each infant. These include:
- heart rate
- respiratory rate
- oxygen saturations
- flow of gas
- PEEP
- fiO2
- humidity temperature
- baby’s position
- nose score- if used on unit
- A blood pressure should be taken at least 24 hourly
- 6 hourly blood pressure should be checked and recorded
- Any agreed changes in CPAP pressure should be documented
4.33 Care of the Nose and Face
Skin Care Policy for Infants Nursed on CPAP
Every hour check visually:
- The generator should be positioned correctly
- The nose should not be squashed or pushed upwards
- The eyes should be clearly visible
- Tapes should not be too tight and should certainly not cause indentation, pitting or ocular oedema
At least four hourly check physically:
- The hat should be checked for tightness and correct fit regularly – it should not be too tight or too loose or rub against the infant’s skin
- Prongs/Mask should be removed from the nose to allow rest from the pressure on it, more often if the infant’s condition dictates
- The nose should be inspected for signs of redness, skin breakdown, bruising, indentation, altered shape and bleeding. Any alteration in appearance should be documented
- Prongs/Mask should be checked to ensure that they are clean and patent, prior to being replaced on the infant
- The ears should be inspected to ensure that they are not creased or folded. They should also be inspected for signs of skin breakdown, redness, bruising, swelling, discharge or bleeding. Any alteration in appearance should be documented
Remember:
- Prongs/Mask should be removed by loosening of the tapes rather than pulling them straight off the infant’s face
- Regular mouth care should be performed
- Suctioning should NOT be routine but as dictated by the infant
- It is important that documentation is completed when the nose is checked and any changes noted
If there are changes to the nose or surrounding area:
- Check that all of the above have been followed – that the hat/mask/prongs are the correct size and are clean and patent. That there is no error with the set-up of the CPAP. Document and recheck in 1-2 hours depending on severity.
- Recheck – have there been any changes? Has it improved or deteriorated? If improved, document and continue to recheck regularly, minimum of every four hours. If deteriorated, inform nurse in charge and medical staff, document.
- Try increasing time off to relieve pressure, consider facial oxygen if needed. Consider using Vapotherm if available or alternating mask and prongs. Consider a dressing or treatment to the affected area. Document any changes in care.
- Consider elective intubation and ett CPAP /ventilation. Inform tissue viability nurse and plastic surgeons. Complete an incident form. Document any changes in care.
Version Control
| Version | Date | Details | Author(s) | Comments |
| 4th | Feb 2018 | Reviewed and updated. | TVWNODN, Quality Care Group.
KR chair |
Approved by the Lead Nurses and Practice Educators Group |
| 5th | June2023 | Reviewed and updated | TVWNODN Guidelines group.
KR chair |
Has been for review- comments received, changes made. Ratified at Governance meeting June 2023 |
| Review Date: | June 2026 | |||
Document version
Version 5
Lead Authors
Thames Valley & Wessex Neonatal Network Guidelines Group
Approved by
Thames Valley & Wessex Neonatal Network Governance Group
Approved on
15 June 2023
Renew date
June 2026
Full guide
Related documents
Alys (2001) Nasal prongs continuous positive airway pressure: a simple yet powerful tool, Pediatrics, 108, pp759-61
Bamat et al (2016) Duration of continuous positive airway pressure in premature infants. Seminars in fetal and neonatal medicine. June; 21(3) pp189-95. Found at; https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4902733/
Bowe.L, Clarke, P (2005) Curent use of nasal continuous positive airway pressure in neonates, Archives of Disease in Childhood, Fetal and Neonatal Ed, 2005, 90, f92-4
CAHS (2021) Continuous Positive Airway pressure (CPAP)
Guideline. Government of Western Australia |Child and Adolescent services, Child and Adolescent health Services. P1-15.Found at:
Continuous Positive Airway Pressure (CPAP) (health.wa.gov.au)
Cahill.S (2012) Continuous Positive Airway Pressure (CPAP) Nursing Guidelines. NHS Forth Valley, version 1, pp1-12.
Chandrasekaran. A et al (2017) Nasal masks or binasal prongs for delivering continuous positive airway pressure in preterm neonates-a randomised trial. European Journal of Pediatrics.
March 176 (3) p379-86. Found at; https://www.ncbi.nlm.nih.gov/pubmed/28091776
Clements.J et al (2023) A randomized trial comparing waening from CPA alone with weaning using heated humidified high flow nasal cannula in very preterm infants: the CHiPS study.Archives of Disease in Childhood, fetal and neonatal addition. Vol 108, F63-68.
De Klerk.RK (2001) The use of continous positive airway pressure in preterm infants, comments and experience from New Zealand, Pediatrics 108, pp761-2.
De Paoli AG, Morley, C, Davis, PG (2003) Nasal CPAP for neonates, what do we know in 2003? Archives of Disease in Childhood, Fetal and Neonatal Ed, 88, f168-72
Fessler.H.E (1995) Effects of CPAP on venous return. Journal of Sleep Research. June 4(S1) pp44-49. Found at; https://www.ncbi.nlm.nih.gov/pubmed/10607172
Goel.S et al (2015) Nasal Mask Versus Nasal Prongs for Delivering Nasal Continuous Positive Airway Pressure in Preterm Infants with Respiratory Distress: A Randomized Controlled Trial. Indian Pediatrics, Dec Vol 52, No 12, pp1035-40. Found at; https://www.ncbi.nlm.nih.gov/pubmed/26713987
Graham.S (2004) Continuous positive airway pressure: the story of change in a neonatal intensive care unit. Journal of Neonatal Nursing, July, 10(4) pp130-4.
Heenan.H (2005) Infants requiring continuous positive airway pressure (CPAP), Clinical Guidelines, Milton Keynes NHS Trust, Milton Keynes.
Ho.T and Mok.J (2003) Condensate clearance from CPAP circuit: an examination of two methods of draining condensate from the inspiratory tubing, Journal of Neonatal Nursing July, 9(4) p117-20
Lamburne.S (2014) An assessment tool for infants requiring nasal continuous positive airway pressure. Infant, Vol 10, Issues4, pp123-6
Liverpool Womens (2011) Guidelines for the use of Nasal CPAP on the Neonatal Unit. Version 3, NICU 32. www.liverpoolwomens.nhs.uk
Morley.C, Davis,P (2004) Continuous positive airway pressure: current controversies. Current Opinion in Pediatrics 16, pp141-45
NICE (2020) Specialist neonatal respiratory care for babies born preterm. NICE Quality Standard. Found at www.nice.uk/guidance/qs193
O’Shea.J and Kirolos.S (2022) Respiratory Management of preterm infant, Greater Glasgow and Clyde NHS, Found at;
Respiratory management of preterm infants (scot.nhs.uk)
QCG (2020) Respiratory distress and CPAP. Queensland maternity and neonatal Clinical Guidelines, page 1-32. Available from http://health.gld.gov.au/qcg
Roberts.C.Tand Hodgson.K.A (2017) Nasal High Flow Treatment in preterm Infants. Maternal Health, Neonataology and Perinatology. Vol 13, No 3, Found at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5586012/
Sabry.A.M et al (20203) Clinical predictors for outcome of continuos positive airway pressure in respiratory distress syndrome in preterms: Single Center Study. Pediatric Sciences Journal, Vol 3, issues 1, pp 1-15. Found at: Clinical Predictors for Outcome of Continuous Positive Airway Pressure in Respiratory Distress Syndrome in Preterms: Single Center Study (ekb.eg)
Sivanandan.S and Jeeva Sankar.M (2020) CPAP failure in neonates: practice, experience, and focus do matter! The Indian Journal of Pediatrics (November 2020) Vol 87, no 11, pp881-2
Stanley.A (2013) Management of an Infant on the Children’s ward with nasal Continuous Positive Airway Pressure Therapy. Mid Essex Hospital Services. Version 2.0, pp1-17.
Van Delft.B et al (2020) Weaning strategies for the withdrawl of non-invasive respiratory support applying continuous positive airway pressure in preterm infants: a systematic review and meta-analysis. BMJ Paediatrics, pp1-8 v4(1) e000858
Wardle.S et al (2010) Continuous Positive Airway pressure
(CPAP) Nottingham Neonatal Service- Clinical Guidelines. Version 2. Pp 1-13.
Yong.SC, Chen.SJ, Boo.NY (2005) Incidence of nasal trauma associated with nasal prongs versus nasal mask during continuous positive airway pressure treatment in very low birthweight babies: a randomised control study. Archives of Disease in Childhood, Fetal and neonatal Ed, 90, F480-483.
Information also gained in conversation with;
- Myles Mylor, Tissues Viability Nurse Consultant, John Radcliffe Hospital, UK
- Philomena Edwards, Clinical Specialist, Viasys Healthcare UK Ltd, Welton Road, Warwick, CV34 5PZ
- Lauren Linder, Clinical Specialist, Viasys Healthcare UK Ltd, Welton Road, Warwick, CV34 5PZ.
Implications of race, equality & other diversity duties for this document
This guideline must be implemented fairly and without prejudice whether on the grounds of race, gender, sexual orientation or religion.