Palliative, End of Life and Spiritual Care Section
The information on this page is intended for health professionals reference and use only. If you are a parent or family member looking for information about treatment, please visit unit information.
Contents
Executive summary
1.0 Introduction
1.1 Scope of guideline
1.2 Purpose of guideline
1.3 Definitions
2.0 Background
3.0 Aspects of Neonatal Palliative Care to Consider
3.1 Establish Eligibility of Baby for Palliative Care
3.2 Planning Palliative Care with Families
3.3 Communication and Documentation
3.4 Flexible Parallel Care Planning
3.5 Pre-Birth Care
3.6 Transition from Active Postnatal to Supportive Care
3.7 End of Life Care
3.8 Post End of Life Care
4.0 Referral for Hospice Care
4.1 Referrals
4.2 Items to Remember
4.3 Children’s Hospices within Thames Valley & Wessex
5.0 Offering Choices and Creating Memories
6.0 Key Points to Remember when Moving to Palliative/Comfort Care
7.0 Key Points for Palliative/Comfort Care at Home
8.0 Guidance for Peri-Mortem Photography and Image Archiving
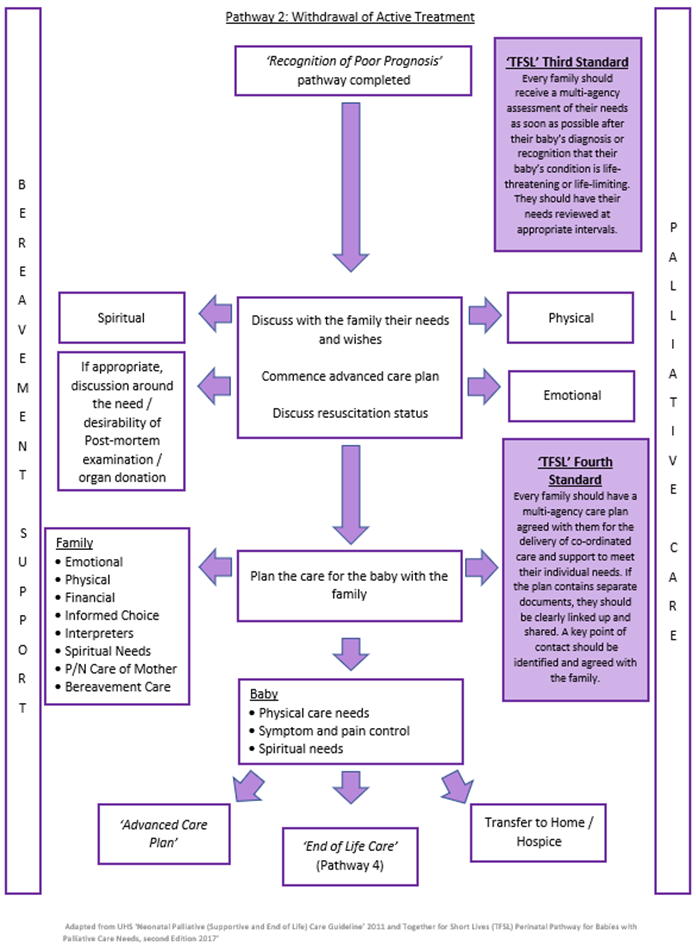
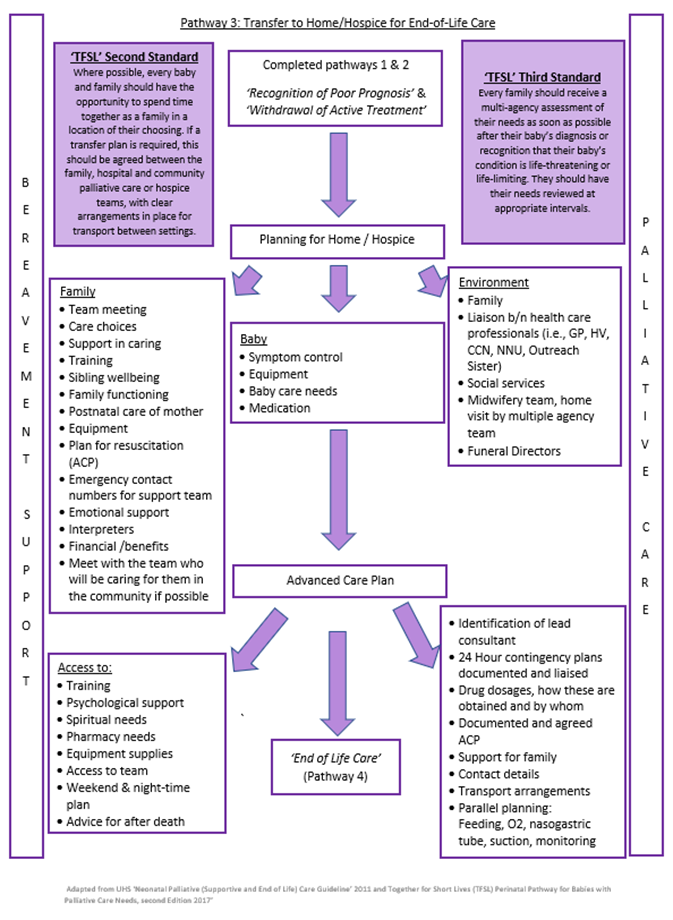
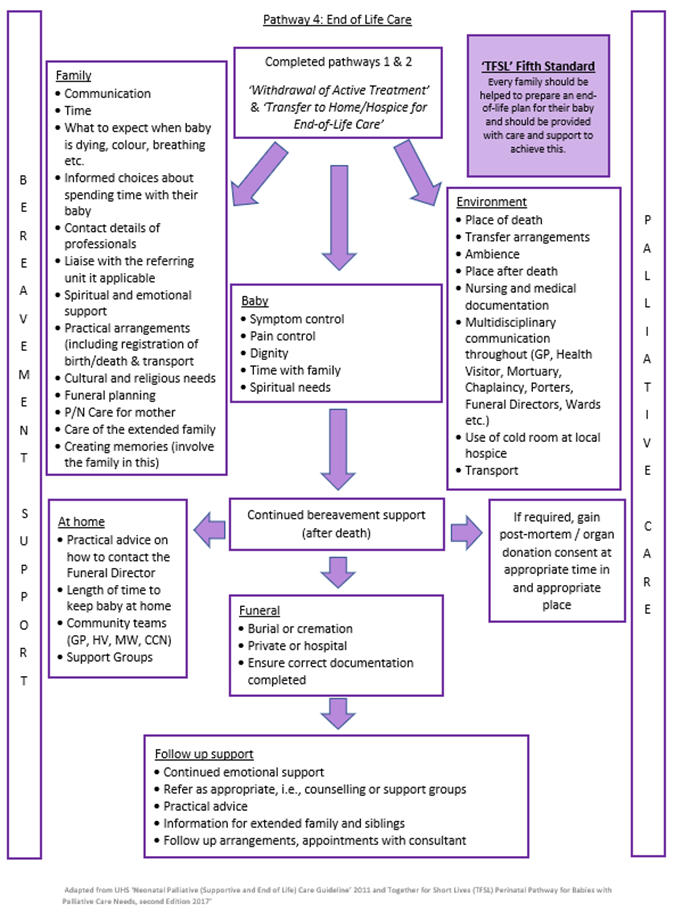
Pathways
Appendix A – Advanced Care Plan Documents
Further Resources
Executive summary
“Palliative care for the neonate with a life limiting condition is an active and total approach to care from the point of diagnosis or recognition, throughout the child’s life, death and beyond. It embraces physical, emotional, social, and spiritual elements and focuses on the enhancement of quality of life for the baby and support for the family. It includes the management of distressing symptoms, provision of short breaks and care through death and bereavement.” Together for Short Lives 2018
This guideline sets out best practice in planning palliative and end of life care for a neonate.
1.0 Introduction
Decisions about end-of-life care planning should be based on the best possible information about the diagnosis and prognosis of the underlying condition. Palliative care should only be considered if the baby has a life limiting condition. Joint decision making with parents, open communication and clear documentation are essential. An individualised care plan should be drawn up after multidisciplinary discussions between the neonatal team, the parents, specialist palliative care and local community teams where appropriate.
The care plan should cover all foreseeable outcomes and should be flexible enough to allow for changes in the condition of the baby or in the parent’s views and wishes.
1.1 Scope
This guideline applies to all neonates cared for within Thames Valley & Wessex Neonatal Network who require palliative care.
1.2 Purpose
To provide guidance for clinical staff on decision making and developing integrated care pathways across Thames Valley & Wessex for neonatal palliative care.
1.3 Definitions
Neonatal palliative care encompasses planning and provision of supportive care/symptom management for however long is required for a baby with a life-limiting/life-threatening condition and their family. This care may continue for months/years.
2.0 Background
Advances in antenatal diagnosis, obstetric and neonatal care, and care at the margins of viability have all increased the need for decision making about end-of-life care for the neonate. Antenatal diagnoses of abnormalities not compatible with life are being confirmed earlier in pregnancy and a plan for palliative care may be needed at any stage, particularly when the diagnosis is made beyond 20-22 weeks gestation. Palliative care may also be needed in the perinatal period for example because of extreme prematurity or following the diagnosis of a condition with a very poor long-term prognosis.
The Nuffield Council of Bioethics (Nuffield 2006) and the British Association of Perinatal Medicine guidance support the decisions of clinical staff and parents not to resuscitate or institute intensive care when this would not be in the baby’s best interests. The RCPCH provides guidance on withholding and withdrawing life sustaining treatment in children, and the GMC document ‘Treatment and Care towards the End of Life: good practice in decision making’ includes a specific section for neonates, children, and young people.
Palliative care planning involves multidisciplinary team planning. Choices in care may vary up until the end of life and there may be a transition into and out of active, supportive and end of life care.
3.0 Aspects of Neonatal Palliative Care to Consider
- Establish eligibility of baby for palliative care
- Family care
- Communication and documentation
- Flexible parallel care planning
- Pre-birth care
- Transition from active postnatal to supportive care
- End of life care
- Post end of life care
3.1 Establish Eligibility of Baby for Palliative Care
Babies may be eligible for palliative care in situations where it is felt that they have such a severe reduction in the future quality and quantity of their life, that life sustaining treatment would not be in their best interest.
These can be categorised as.
A. Antenatal diagnosis of severe congenital abnormality.
B. Extreme prematurity.
C. Post-natal illness or complications.
The prognosis should be agreed by at least two senior clinicians. (Neonatologist/Surgeon/Cardiologist/Neurologist/Geneticist/Paediatrician, as appropriate)
Palliative care should only be considered when the diagnosis is confirmed antenatally or postnatally by genetic testing, scans or other investigations, and a multidisciplinary team has agreed the diagnosis and prognosis (not essential in conditions with simple definitive tests and agreed prognosis e.g., anencephaly).
The prognosis should then be explained and discussed with the family. If either the parents or staff members are still uncertain about the diagnosis or prognosis a second opinion, either internal or external, should be sought. There are circumstances where palliative care may appropriately coexist with active management, particularly in the face of uncertainty.
3.2 Planning Palliative Care with Families
3.2.1 Communication
- Families will require support at many levels. Parents will be shocked, frightened, and stressed by the knowledge that their baby has a life limiting condition or abnormality not compatible with life. They may also be grieving for the loss of a normal pregnancy and birth and a planned for and dreamed of future. Parents of twins and other multiples may have to cope with additional complex and conflicting emotions, for example dealing simultaneously with end-of-life care for one baby whilst remaining hopeful and optimistic for another. Parents in these situations are likely to be both emotionally and physically exhausted. They may have other children to care for and may be travelling long distances to visit their baby. All the above make it difficult for parents to understand and take in complex and distressing information.
- When planning palliative care, it is essential that there should be multidisciplinary discussions involving the parents, a senior clinician experienced in paediatric/neonatal care and where possible a neonatal nurse/midwife involved with the care of the baby (minimum). The discussion must be conducted in a quiet and private setting and the family should be offered the opportunity of a third party being present to support them.
- The parents should be given time to assimilate information and time to discuss it with their wider family or friends if they wish to. Further discussion should be offered.
- The phrase ‘withdrawal of care’ should be avoided and ‘palliative, comfort care or withdrawal of intensive care treatment’ should be offered.
- An interpreter should be available if required, as it is essential that the parents have a full understanding of what is being discussed. Family members, friends and siblings should not normally be used unless no alternative is available. If families insist on a relative translating, the difficulties with using family members must be explained and documented in the patient notes. Access to Communication can translate written information into other languages and in Braille if required.
3.2.2 Psychological Support
Many parents will be grateful if staff suggests they start to create and collect mementos. These will give some tangible evidence of the baby’s existence and their time together and can be very important in the months and years to come.
Staff should consider whether the family, including siblings should be offered the opportunity to see a trained counsellor. General Practitioners, the primary care team/hospice service may be helpful in providing general support, symptom relief and access to specialist counselling. Parents should be offered written information about the relevant voluntary organisations and support groups such as BLISS, SANDS. Child Bereavement UK and Contact a Family.
3.2.3 Spiritual Support
Parents should be offered a choice of whether they would like to have a religious or spiritual ceremony. Their wishes should be documented in the notes to avoid the same question being asked multiple times.
Ensure clear handover of this information with shift changes. Care should reflect personal, cultural, spiritual, and religious wishes.
3.2.4 Social Support
Written information should be made available for parents informing them of what benefits and support they are entitled to. If parents are entitled to discounted parking and meals, they need to be informed.
SANDS Guidelines for Professionals, 4th Edition: www.uk-sands.org (For staff information regarding benefits)
3.3 Communication and Documentation
3.3.1 Planning Care of the Baby While Alive with Parents
- This refers to the period before a baby dies. This period can range from hours or days to weeks (typically but may be longer). Care of the baby’s needs to be planned to include the approach to resuscitation, nutrition, pain relief and comfort care. The appropriate place for this care should be discussed, and what support the family will need.
- Give the parents choices of how they would like to spend time with their baby as they will rarely have any idea of what they can or want to do and will often look to staff for advice. Ask if they wish to be with their baby, some don’t but may find this difficult to verbalise. It is important their wishes and needs are respected.
- Parents should be offered a copy of the BLISS leaflet ‘Making critical care decisions for your baby’.
- Manage parent’s expectations and assure facilities are available before offered.
3.3.2 Advance Care Plan
- Any baby being discharged home or to a hospice for palliative care must have an Advance Care Plan completed and agreed. This includes resuscitation guidance, what to do in the event of an acute deterioration, wishes of the family and contact details of key members of staff. It must be printed and disseminated to the appropriate people. Parents should always keep a copy.
- If the team making these decisions with the family are not local to where the baby will receive care the outcome of these discussions must be communicated as soon as possible to the local team who will be caring for the family. Parental consent should be obtained for this.
- It is vital to involve or inform members of the Specialist Palliative Care Team, Primary Care team/hospice service about palliative care planning as soon as possible as they may be part of the team delivering palliative care and will provide ongoing support to the family.
- Ensure all therapists involved are aware of the plan to move to palliative care.
- At all times the parents should have the name and contact details of a key member of staff.
3.4 Flexible Parallel Care Planning
Whilst there are many situations where there is a reasonable certainty of death during fetal and neonatal life, there are babies who survive longer than expected during supportive and end of life care.
It is vital that care planning is continuously reviewed in the best interests of the baby. There should be parallel planning for transition periods into and out of active, supportive and end of life care. Any changes should be well documented and communicated.
3.5 Pre-Birth Care
When a diagnosis of a life-limiting condition is made antenatally it may be appropriate for palliative care planning to begin prior to the birth of the baby. A senior clinician (neonatal/surgical/cardiologist etc) Specialist Palliative Care Team and nursing/midwifery staff should be involved in creating a palliative care plan for the baby with the family. This should include an approach and limitations to resuscitation at birth and location of ongoing care.
3.6 Transition from Active Postnatal to Supportive Care
In some situations, a rapid assessment by a senior clinician may be needed to confirm a candidate condition for palliative care. Occasionally specific tests may be helpful e.g., rapid karyotype of cord blood in the case of anomalies suggestive of life limiting chromosomal abnormality.
3.7 End of Life Care
3.7.1 Predicting the Time of Death
A baby with a serious or life limiting abnormality diagnosed during pregnancy may die at any time during pregnancy and through to infancy. For some babies it can be very difficult to predict a time of death. The multidisciplinary team should discuss the possible or likely timing of death and any uncertainties with both parents and staff. Parents and staff should be informed as soon as possible of any changes.
3.7.2 Location of Care and Death
Depending on the situation and the level of support required the baby might die on the delivery suite, on a postnatal ward, in the neonatal unit, at their local hospital, at home or in a children’s hospice. The lead clinician should discuss with the parents where the baby will be cared for, explain what is likely to happen and take their wishes into account as far as possible. If a baby is being transferred home or to a children’s hospice, the mother’s health must also be considered and planned for, where possible transport should be arranged to allow time at home or at the hospice prior to the period of end-of-life care Involve the Palliative Care team as soon as possible for support and advice.
3.7.3 Physical Comfort Care
Continue to practice basic care to minimise distress; positioning, skin care, mouth care, human contact including breast feeding (if appropriate), and skin-to-skin contact. If the baby is comfortable temperature does not need to be monitored. Developmental needs should not be forgotten.
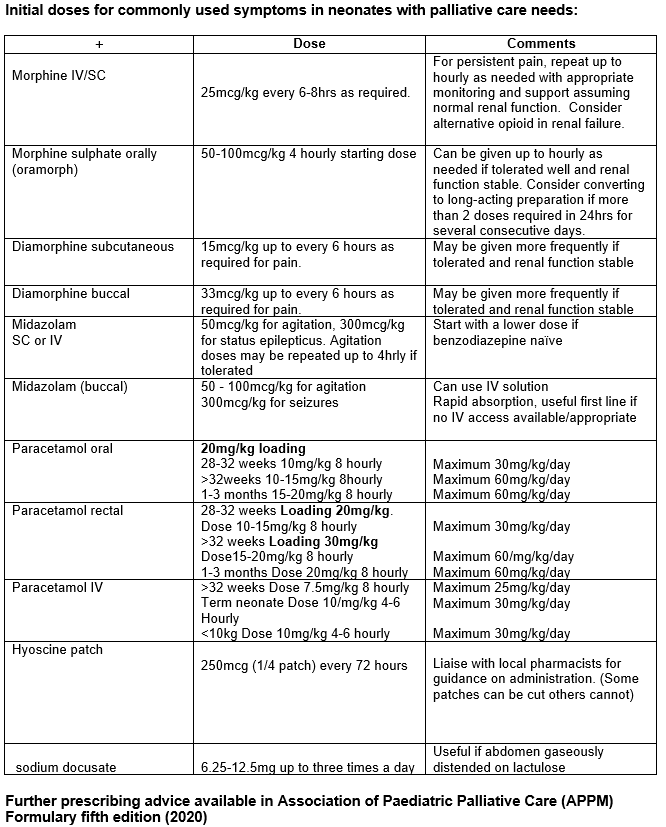
3.7.4 Pain, Distress and Agitation
Assess and treat any underlying causes of pain. Consider paracetamol. If not sufficient, use morphine via the route best tolerated by the baby (oral, buccal, intravenous, or subcutaneous) There is no limit to the dose of morphine for relief of pain or distress. Recent research in palliative care shows that morphine titrated to symptoms as part of palliative care does not hasten death. Midazolam may also be used and is particularly helpful if seizures are a feature or agitation is prominent. Symptoms should be managed by teams confident in managing symptoms in neonates with palliative care needs. For complex cases the University Hospitals Southampton Paediatric Palliative Care Team should be contacted for advice. Please see the Association of Paediatric Palliative Medicine Master Formulary for dosing and conversion from ‘as required’ dosing to longer acting medications.
This is available for free from: https:/www.appm.org.uk/guidelines-resourses/appm-master-formulary/
Specialist Symptom Management Advice is available from:
University Hospitals Southampton Specialist Paediatric Palliative Care Team.
Dr Kate Renton, Palliative Care Consultant. Kate.renton@uhs.nhs.uk Dr Tim Warlow. Palliative Care Consultant. Tim.warlow@uhs.nhs.uk
Julia Whatley. Paediatric Palliative Care Nurse Specialist. Julia.whatley@uhs.nhs.uk
Helen and Douglas House
Dr Emily Harrop, Paediatric Palliative Care Consultant. eharrop@helenanddouglas.org.uk
Dr Charlotte Holland, Consultant Paediatrician with a Special Interest in Paediatric Palliative Care. clholland@helenanddouglas.org.uk
3.7.5 Nutrition, Feeding and GI Symptoms
The goal of feeding is to provide comfort and reduce distress from hunger with growth as a secondary outcome. The route of feeding should be what is most suitable for the baby. Parenteral fluids and nutrition and nasogastric feeding are rarely indicated. Breast feeding may be comforting for the baby and mother.
- Vomiting: Consider reducing feed volume and the use of anti-reflux treatment if symptomatic.
- Constipation: May be caused by opiates. If causing distress use lactulose or sodium docusate, (fewer problems with wind related distension) or glycerine suppositories.
- Urinary retention: May be caused by opiates. Consider abdominal pressure and rarely catheterisation.
- Respiratory secretions: Should only be treated if causing distress to the baby. Consider hyoscine patches.
3.7.6 Investigations, Monitoring and Treatment
Monitoring is not necessary but may be used if helpful to parents. Investigations should only be performed if the results might lead to treatment that will improve the baby’s quality of life or help with the diagnosis and management of subsequent pregnancies. Treatments such as oxygen, anticonvulsants, anti-reflux medication may all have a role in symptom control.
Immunisations should be given as per national immunisation programme unless contra-indicated.
3.7.7 Resuscitation Plans
Limitations to resuscitation should be discussed, documented, and regularly reviewed. Comfort and dignity of the baby should be maintained. The CYACP (Child and Young Persons Advanced Care Olan) should be used for this.
3.7.8 Changes in Appearance of the Dying Baby
Staff should explain to parents the physical changes that are likely to occur as their baby dies and should discuss with them whether they want to see and hold their baby whilst dying or after death. Terminal gasping should be explained to reassure parents that this is not an indication of suffering. (Refer back to 3.7.4) Parents should be made aware that the time until death can vary from minutes to hours and sometimes days or longer. It is important to assure parents that there will be frequent reviews of their babies needs when on a palliative care pathway.
3.7.9 Post- Mortem Examination
Discussions about post-mortem examination can begin prior to a baby’s death if felt appropriate and consent may be sought at this stage, particularly if the family plan to leave hospital. A senior, trained member of staff should sensitively discuss post-mortem examination so that maximum information can be obtained.
This may confirm the diagnosis and provide information, which may help the parents to come to terms with their loss. However, parents should be informed of the possibility that the review may not always give a clear cause of death.
Information gained may also be important when the parents think about another pregnancy. The coroner should be informed about any death where the cause is unknown or uncertain, within 24 hours of any operation or within one year of a major operation. The coroner’s officers are happy to discuss cases and give advice. Results may not be available for 10 – 16 weeks. It may be helpful to mention that if a specific neuropathological examination is required, there may be a significant delay in the baby being ready for burial or cremation. Where religious faith dictates the need for early burial/cremation it may be possible to return the body without nervous tissue, which can then be buried/cremated later. Discuss individual cases with pathologists.
3.7.10 Organ & Tissue Donation
Organ donation is possible after diagnosis of death by cardiovascular criteria. This usually occurs in the setting of withdrawal of life-sustaining treatment. It is also sometimes possible in infants with antenatally diagnosed severe congenital abnormalities who die shortly after birth.
Organ donation can also occur in infants after diagnosis of death by neurological criteria (i.e., ‘brain death).
In either of these situations, if there is a possibility that an infant may be eligible for organ donation, particularly if families have expressed an interest in donation, clinicians should contact and discuss their local Specialist Organ donation team – prior to withdrawal of life-sustaining treatment.
There are currently no lower limits set on age or weight. Referral has been accepted from a 36 week’s gestation, and organs have been transplanted from a 1.9kg donor.
Heart valves can be donated from 32 weeks gestation and a lower weight limit of 2.5kg.
The baby’s body needs to be in the mortuary or cold cot within 6 hours of death. There can be some flexibility around this, but it decreases the time the team would have to retrieve the valves.
It is not possible for neonates to donate corneas or skin.
Brain Stem death testing: There is guidance for testing babies between 37 weeks gestation and two months. New guidance can be found here: The diagnosis of death by neurological criteria in infants less than two months old. April 2015.
In case of query please contact the Organ Donation Team:
Refer by regional pager 07659183499 For Organ donation,
Tissue donation: 08004320559.
The team run a 24-hour on call service and are happy to advise at any time, they will also come and discuss options with families where appropriate.
3.8 Post End of Life Care
- Local guidelines and paperwork should be completed.
- Inform families about registering the birth and death, funeral arrangements, and sources of ongoing support.
- Child Death Overview panel (CDOP) paperwork will also need to be completed electronically (All baby deaths)
- MBRRACE (All babies 28 days and less)
- PMRT (All babies)
3.8.1 Certification and Registering of Death
If a baby is born with signs of life before 24 weeks, is stillborn at or after 24 weeks, or is born alive and subsequently dies, the parents must register the stillbirth or birth and death. They should be given verbal and written information about how and where to do this, together with information about arranging a funeral.
A doctor who has seen the baby within the past 28 days and is certain about the cause of death can sign the death certificate. Doctors signing death certificates should have received training in completing a certificate. When an expected death occurs at home there is no urgency for the family to call a doctor. The Advance Care Plan (ACP) should indicate who and when to inform when a baby dies at home. If a family calls an ambulance when a baby dies, the police are automatically informed unless they have an ACP. The ACP is particularly important at this point and parents should keep a readily available copy at their home.
In the case of a Coroner PM, a medical certificate of death cannot be issued by medical staff; it will be issued from the coroner.
The Coroner‘s Officer will contact the family directly to inform them of the process that will take place, i.e., with regards to the baby’s registration of death and the need for an inquest if a cause of death cannot be found at post-mortem.
3.8.2 Muslim Funerals
For Muslim families it is important for the funeral to take place as soon after death as possible to avoid embalming or otherwise disturbing the body of the deceased.
- Be aware of local Funeral Directors who arrange Muslim funerals.
- Generally following the registration of birth/death, the Mosque funeral director will accompany the family to the Bereavement services office. Here the necessary paperwork is completed to allow the funeral to happen that day if possible.
- In some areas baby graves are pre dug and locked so they are easily available.
- Muslim babies are usually buried in designated areas.
- Muslim babies cannot be buried at a weekend or on Bank Holidays, as generally Bereavement Services Offices are not open. (Please check locally) Therefore, this would be organised for the next available working day. Other district offices may work differently. If babies need to go out of area for burial, the baby must still be registered in the normal way and can be done by contacting the out of hours Registrars Number if needed out of office hours.
- Parents may wish to contact the Mosque and Imam themselves. Please ask what their wishes are.
- If this is the case, the Imam will organise everything including the registration.
3.8.3 Alternative Religions
A reference file should be available listing procedural variances required for specific religious groups. This will ensure the individual spiritual needs are met for all families.
3.8.4 Communication and Follow-Up
Staff should ensure the mother’s GP and the local primary care team/hospice service are informed about the baby’s death so that they can offer ongoing care and support and sign- post parents to local support. Staff should check they have contact details of the relevant charities that offer care and support to bereaved parents such as SANDS, BLISS, and the Child Bereavement UK.
Support websites:
- www.uk-sands.org
- www.childbereavement.org.uk
- www.simonsays.org.uk
- www.tcf.org.uk
- www.crusebereavementcare.org.uk
- www.careconfidential.com
Parents should be offered a follow up appointment to have the chance to discuss their child’s problems and care. The timing of this may vary depending upon the availability of outstanding investigations including the post-mortem, or the parent’s needs and wishes. More than one follow- up contact may be appropriate. Co-ordinating follow up between specialities can be helpful in minimising visits for the family.
3.8.5 Taking a deceased baby home
There is no legal reason why parents may not take their baby out of the hospital at any gestation. However, for the protection of the parents and to avoid misunderstandings, staff should give parents documentation to take with their baby’s body and advice about caring for the baby’s body and contacting the Funeral Director within 24 hours of arriving at home. (The exception to this being if the baby is the subject of a Coroner case).
4.0 Referral for Hospice Care
4.1 Referrals
Hospices accept referrals for infants who have a life limiting or life -threatening condition and require palliative care, symptom management and support. These can be made antenatally. Early involvement of the Specialist Paediatric Palliative Care Team is advisable for support and advice in planning end of life care and the options the family would have.
They accept urgent referrals for end-of-life care for infants who have not been previously known to them and are able to ‘fast track’ these referrals to ensure families can visit as soon as possible. Some hospices can visit the unit to meet the parents and offer symptom management support to the team or provide retrieval support.
Routine referrals can be made for infants expected to live for a while. The hospice may be able to offer a ‘stepped discharge’ and ongoing respite and support. Each infant is assessed, and medical information gained from the child’s or young person’s consultant. Usually, this information is then discussed at clinical committee – this can take a few weeks.
(Referrals can be made by telephone with the appropriate hospice listed in 4.3.)
4.2 Items to Remember
- Some of the hospices like to visit/meet the parents prior to the transfer agreement, facilitate this if required.
- Completed Rapid Transfer Documentation.
- All current & possible medication/dressings including Controlled Drugs & Anti-convulsant must be provided (they may not stock all medication). When writing controlled drugs on TTO form all requirements including dosage and volume must be written in words NOT figures/numbers.
- Syringe Drivers.
- Any enteral feeding? If so, do they have a supply?
- Full history & care plan – including any special requirement/wishes from the parents.
- Clear plan from lead consultant to go with the infant.
- Who will be staying with the infant?
- Has the baby been registered? If not, father will not be able to complete the paperwork on his own following the infant’s death.
Additional information is available on the websites listed below.
4.3 Children’s Hospices within Thames Valley & Wessex
A list of all children’s hospices can be located on the ‘Together for Short Lives’ website: http://www.childhospice.org.uk/home.aspx
HAMPSHIRE
Naomi House
Stockbridge Road
Sutton Scotney
Winchester
Hampshire
SO21 3JE
www.naomihouse.org.uk
Telephone: 01962 760555
WEST SUSSEX
Chestnut Tree House Children’s Hospice
Dover Lane
Poling
West Sussex
BN18 9PX
www.chestnut-tree-house.org.uk/
Telephone: 0845 450 5820
DORSET
Julia’s House
35 Springdale Road
Corfe Mullen
BH18 9BP
www.juliashouse.org/
Telephone: 01202 389837
Surrey
Shooting Star Children’s Hospice
Old Portsmouth Road
Artington
Guildford
GU3 1LP
Telephone: 01483 230974
familysupport@shootingstar.org.uk
Thames Valley
Helen & Douglas House
14a, Magdalen Road
Oxford
Oxfordshire
OX4 1RW
www.helenanddouglas.org.uk
Telephone: 01865 794749
Rennie Grove Peace Hospice Care
52a Western Road
Tring
Herts
HP23 4BB
http://www.irhh.org/sitehome/ournursingservices/children/index.html
Telephone: 01442 890222
Alexander Devine Children’s Hospice Services
Snowball Hill
Woodlands Park Ave
Maidenhead
SL6 3LU
www.alexanderdevine.org
Telephone: 01628 822777
5.0 Offering Choices and Creating Memories
It is important for parents to think carefully about how they would like to spend time with their baby. They have so little time as a family, so it is important that they make decisions that will not leave them with regrets.
It’s important they know this is all the time they have.
Parents may have no idea how they would like to spend time with their baby or what may be possible.
Therefore, as staff we need to guide them and offer choices and respect their wishes and decisions.
This is not a prescriptive list. Please listen to the parent’s wishes and needs.
Things they may like to consider:
Spending Time and Creating Memories with their baby.
- Spending time with their baby before and after death, as a family and in privacy. Ambience is an important thing to consider.
- Choosing clothes for a religious service if there is to be one. Taking photographs of that service. Remember My Baby could be offered to parents. If available locally. https://remembermybaby.org.uk/
- Encourage them to spend as much time as possible with their baby, even before a move to comfort care.
- It’s okay for them to sit and read to their baby.
- Involving other family members if they wish to.
- Photographs with siblings, family, and friends. With a twin if possible. Encourage parents to capture all the moments in the time they have together, i.e., washing, dressing the baby.
- Mementos they may like to keep or things they wish to stay with their baby. Encourage siblings, where appropriate, to draw pictures for the baby.
- Create a memory box/journey for the siblings if that’s appropriate.
- Ask what they would like to keep. Don’t assume.
- Offer hand and footprints and moulds. Parents may wish to help with the footprints. Carefully explain what the moulds are, tiny hands and feet, not just impressions.
- They may wish to bring in their own home comforts to have around them. Again, thinking of the ambience.
- It may be appropriate to offer the parents the choice of transferring their baby home to die. This would need to be discussed on an individual basis before being offered
- Consider transfer to hospice for end-of-life care. This needs to be discussed with the Hospice team before approaching the family.
Following their baby’s death.
- They should be allowed time and not feel rushed.
- They may wish to spend the night with their baby with them.
- They may like to take their baby home, for a short time or until the funeral director takes the baby for them.
- They may like to take their baby for a walk or spend some time out of the Neonatal unit environment.
- They may have a special place they wish to share with their baby.
- They may wish to see their baby again. Choices should be offered, and requests facilitated.
- Time is important. DO NOT rush parents into making decisions regarding funerals or PM request at the time of death. It may be appropriate to have discussions before death, or after the parents have had time to assimilate what is happening to them. Ideally in the following day or two. Parents may need to return to the hospital for documentation to be completed and should be made aware of that, but also the importance of taking time with their decision making.
- They may wish to discuss decisions with their extended family.
- Parents may have wishes of their own and they should be encouraged not to be afraid to ask staff and for staff to help them achieve this, if possible.
- Consider transfer to hospice following death. Discussion with Hospice needed before approaching family with this suggestion.
Remember this is all the time parents have.
They will not have this time again.
These are all the memories of their baby they will ever have.
Nothing is a silly request.
TIME AND CHOICE are the words to remember.
6.0 Key Points to Remember when Moving to Palliative/Comfort Care
- Ensure information is gathered and shared about the baby with family.
- Professionals need to be open and honest with families.
- Explore the concerns and feelings of all family members, including extended family, if appropriate.
- The needs of the baby and family should be assessed as soon after diagnosis as possible. This assessment needs to be made in partnership with the family.
- Joint planning with families and professionals should start as soon as possible.
- Commence ACP to document families’ wishes and discussions around limitations to resuscitation.
- If appropriate discuss with mum suppression of lactation and offer information regarding breast milk donation. (Framework for Practice: Lactation and loss | British Association of Perinatal Medicine)
- Assess all medical, nursing, practical, social, psychological, and spiritual needs.
- Aim to reach an understanding of the individual situation and the impact that situation has on the family.
- Explore, before meeting with the family, all local options available.
- Ensure an agreed and documented plan for care/intervention.
- The baby must be kept as central in the process; however, care should be taken to include the needs of the whole family.
- The family’s religious, cultural, and personal beliefs should be respected.
- Information should be gathered and recorded systematically, to ensure consistency.
- Information sharing is important and full and frank handover of care is essential.
- Straightforward language should be used. Avoid medical jargon.
- Confidentiality and consent should be addressed.
- It may be appropriate to introduce the subject of Post-Mortem examination at this point if felt appropriate. Staff with appropriate skills and local knowledge must make assessments and take consent. Generally, this would be the Consultant Lead. Give relevant written information as required.
- It must be made clear who is taking the lead role.
- Staff involved in the care of the families should have their own access to support and supervision.
- Ensure that six week follow up is offered.
- Communication checklist should be completed and signed as soon as possible to ensure all appropriate persons are notified.
- Ensure families are offered verbal and written advice and information about contact details of support available to them after they have left the neonatal unit.
7.0 Key Points for Palliative Care/Comfort Care at Home
The Specialist Paediatric Palliative Care Team should have met the family and been informed of their discharge to home. A named Neonatal Consultant must be assigned to the family.
- All babies receiving palliative/ comfort care at home should have an agreed ACP, with verbal communication and copies sent to the relevant people.
- Every family should have a key worker to co-ordinate their plan. This may be the named nurse/Neonatal Home Teams/ Community Nursing Team/ Hospice team.
- Community Children’s Nurses/Hospice outreach team will continue to have a supporting role with the family.
- Information must be made available to the family.
- The plan should include the whole family and take account of the baby’s symptoms and personal care. It must include psychological care of the family, siblings, and baby.
- A 24-hour plan must be put in place and agreed to by the senior clinicians and nursing teams. This should include drug dosages, prescribing and obtaining medications, all contact details, transport arrangements and support available. There must be 24-hour access to pain and symptom control, and a written symptom control care plan.
Also include:
Feeding Documentation regarding comfort or demand feeding
NGT/PEG Feeding with full plan and management of tube if appropriate
Suction Frequency and equipment needed/provided.
Monitoring Saturations/apnoea etc if appropriate.
- If the baby is still alive in 2 weeks, consider the offer of a senior clinician visit at home. This could be a joint visit with the local Palliative Care Lead.
- The family should be able to request a review at any time and the baby and family needs will require ongoing assessment.
- The multi-disciplinary team must assess their effectiveness and co-ordination daily when delivering care.
- Ensure family is given extra support at time of death or if there is crisis.
- Ensure discussions with family have taken place and have been documented around their wishes following the death of their baby. BE AWARE families may change their minds and this should, as far as possible be accommodated.
- If there are any changes to be made to the care, a new care plan (ACP) must be agreed and documented.
8.0 Guidance for Peri-Mortem Photography and Image Archiving
- Images are taken for the benefit of parents.
- Any photography should be undertaken with their consent (verbal is adequate given the circumstances. Please document in body of the notes).
- When taking photos avoid being too intrusive.
- Images of an ill or dead baby often appear better in black and white.
- Suggest taking images of hands and feet (perhaps holding a parent’s finger or soft toy).
- If possible, to prevent images being washed out, switch off the flash and use the room lighting instead.
- Photos maybe saved to disc or USB pens with parental consent.
Remember My Baby; Remembrance photography is available in this area. They can be contacted through www.remembermybaby.org.uk
Pathways

Appendix A
Advance Care Plan Documents
The Advance Care Plan
Child and young person’s ACP Collaborative.
All necessary paperwork and guidance can be found here.
http://cypacp.nhs.uk
Further Resources
- APPM Master formulary fifth edition (2020) – via APPM
https://www.appm.org.uk/guidelines-resources/appm-master-formulary/
- Basic Symptom Control in Paediatric Palliative Care (2022) 10th Edition Via T4SL website
- Palliative Care Toolkit (local) – via Helen & Douglas House website
hdh_palliative_care_toolkit-1.pdf (helenanddouglas.org.uk)
- Clinical Supervision (Staff Support) Toolkit (Local) – via Helen & Douglas House website
hdh-clinical-supervision-toolkit.pdf (helenanddouglas.org.uk)
- Buckinghamshire Healthcare NHS Trust, ‘Heart Valve Donation Following Perinatal Death’ guideline – a copy of this is available from the Neonatal Network tv-w-neonatalnetwork@nhs.net on request
- Together For Short Lives: Perinatal Pathway for Babies with Palliative Care Needs (2017)
https://www.togetherforshortlives.org.uk/resource/perinatal-pathway-babies-palliative-care-needs
- Neonatal Palliative Care for Nurses. (Springer 2020) NICE Guidance NG 61: End of life care for infants, children and young people.
https://www.nice.org.uk/guidance/ng61
Version Control
| Version | Date | Details | Author(s) | Comments |
| 1 | Oct ‘12 | Final | LL | Board Approved |
| 2 | Oct ‘15 | Review/updated | LL | TV&W Neonatal Governance Group approved with agreed amendments. |
| 3 | May ‘19 | Review updated | LL | TV&W Neonatal Governance Group approved with agreed amendments. |
| 4 | May 22 | Review Updates | LL | TV&W Neonatal Governance Group approved with agreed amendments
Regional Paediatric Palliative Care Team |
| Review Date: | May 2025 | |||
Document version
Version 4
Lead Authors
Thames Valley & Wessex Neonatal ODN Palliative Care Group
Approved by
Thames Valley & Wessex Neonatal ODN Governance Group
Approved on
June 2022
Renew date
June 2025
Full guide
Related documents and references
Palliative Care (supportive and end of life care). A framework for clinical practice in Perinatal medicine.
BAPM Working Group Report 2010:
http://www.bapm.org/media/documents/Palliative Care Report final Aug10.pdf
Final Document:
http://www.bapm.org/media/documents/Palliative care final version Aug10.pdf
Critical Care Decisions in Fetal and Neonatal Medicine: Ethical Issues. Nuffield Council on Bioethics 2006:
http://www.nuffieldbioethics.org/neonatal-medicine
The Management of Babies Born Extremely Preterm at Less Than 26 Weeks Gestation: A Framework for Clinical Practice at the Time of Birth. BAPM 2008:
http://www.bapm.org/media/documents/publications/Approved manuscript preterm final.pdf
A Neonatal Pathway for Babies with Palliative Care Needs. Together for Short Lives 2017:
http://www.togetherforshortlives.org.uk/
Treatment and Care Towards the End of Life: Good Practice in Decision Making. GMC 2010:
http://www.gmc-uk.org/static/documents/content/End_of_life.pdf
Making Critical Care Decisions for Your Baby. BLISS:
http://www.act.org.uk/core/core_picker/download.asp?id=446
A care pathway to support extubation within a children’s palliative care framework:
http://www.act.org.uk/page.asp?section=406§ionTitle=A+care+pathway+to+support+extubation+within+a+children’s+palliative+care+framework
Royal College of Paediatrics and Child Health. (2015). Making decisions to limit treatment in life-limiting and life-threatening conditions in children: a framework for practice.
http://doi.org/10.1136/archdischild-2014-306666
The diagnosis of death by neurological criteria in infants less than two months old. April 2015
http://www.rcpch.ac.uk/system/files/protected/page/DNC%20Guide%20FINAL.pdf
UK Paediatric & Neonatal Deceased Donation A Strategy Plan. (2018- 19)
paediatric-and-neonatal-deceased-donation-strategy-final.pdf (windows.net)
Child Death Review. Statuary and Operational Guidance (England) October 2018. (Last updated September2019)
www.gov.uk/government/publications/child-death-review-statutory-and-operational-guidance-england
Mother & Babies: Reducing Risk through Audits & Confidential Enquiries Across the UK. (MBRRACE)
MBRRACE-UK: Mothers and Babies: Reducing Risk through Audits and Confidential Enquiries across the UK | NPEU (ox.ac.uk)
Perinatal Mortality Review Tool
Frequently Asked Questions | NPEU > Perinatal Mortality Review Tool (ox.ac.uk)
Framework for Practice: Lactation and loss | British Association of Perinatal Medicine
www.bapm.org
Remember My Baby:
https://remembermybaby.org.uk/
NICE Guidance NG61 End of Life Care for Infants, Children and Young People)? (has specific Neonatal / antenatal guidance and research recommendations)
Implications of race, equality & other diversity duties for this document
This guideline must be implemented fairly and without prejudice whether on the grounds of race, gender, sexual orientation, or religion.