Respiratory Section
The information on this page is intended for health professionals reference and use only. If you are a parent or family member looking for information about treatment, please visit unit information.
Contents
1.0 Aim of guideline
2.0 Scope of guideline
3.0 Guideline summary
4.0 Background information
5.0 Practice guidelines
5.1 Commencing nHFT
5.2 Ongoing care
5.3 Weaning nHFT
5.4 Positioning
5.5 Tubing
5.6 Nasal prongs
5.7 Flow
5.8 Accessories
5.9 Humidification temperature
5.10 General care
5.11 Automated Oxygen Titration through nHFT device
5.12 nHFT transfer unit
5.13 Parents
5.14 Documentation
5.15 Problem solving
5.16 Ceasing nHFT
5.17 Care of the nose and face
6.0 Appendix – Useful links to videos showing how to set up nHFT systems
1.0 Aim of guideline
To provide a framework to ensure that all infants receiving Nasal High Flow Therapy (nHFT) are optimally cared for.
2.0 Scope of guideline
The guideline applies to all infants receiving nHFT within Thames Valley and Wessex Neonatal Network. See below.
These guidelines have been produced to direct nursing staff in their care of infants receiving nHFT and are based on research findings and agreed current best practice. For accessibility, the guidelines have been collated under distinct subheadings, in the order that information is likely to be needed in practice. However, the reader is strongly advised to read the guidelines in full and to seek the advice and support of more senior or experienced colleagues in the practice setting.

3.0 Guideline summary
- Infants receiving nHFT should be nursed in a safe environment, with access to suction, oxygen and resuscitation equipment at the bedside. Continuous heart rate, respiratory rate and oxygen saturation monitoring should be in place.
- When commencing nHFT the gas flow rate, and FiO2 should be set up in discussion with the medical team, and as directed by local guidelines. Commencing the gas flow rate around 4-6 L/min is common practice, with the oxygen set at the infant’s current requirement.
- Select the correct size of nasal prongs designed for use with the machine that will be used for nHFT. See manufacturers guidance charts. Prongs should be positioned correctly so that the eyes are not obstructed, and the nose is not squashed, and there should be regular inspection for signs of redness, skin breakdown, bruising or indentation, including the mucosa inside the nostrils.
- nHFT circuits should be humidified at all times using a bag of sterile water. Set the temperature to 37°C.
- The infant should have an oro-gastric tube (OGT) in situ and the stomach aspirated at least 4 hourly- to aid in the prevention of abdominal gaseous distention.
- Where available, weaning/ ceasing the nHFT should be according to local written weaning protocol and is usually discussed jointly between the nursing and medical teams.
- nHFT prongs and nHFT circuits are for single patient use and should be changed as per manufacturer’s guidelines and recommendation. Usually weekly for prongs and from every 1-4 weeks for circuits.
- If an infant requires nebulised medication, adaptors are available that enable ‘inline’ nebulisation.
- nHFT may be an uncomfortable and possibly painful experience for infants, so staff should be vigilant for signs of pain and discomfort or distress.
- If the infant is stable, parents/carers should be encouraged to cuddle and/or have skin to skin care with their infant. Sucking feeds may also be possible- discuss with the medical team.
- One hourly observations should be performed and recorded for each infant. These include; heart rate, oxygen saturations, transcutaneous pO2 and pCO2 if in use, flow of gas, fiO2, humidity temperature, skin checks (nose/ face), infant position.
4.0 Background information
The use of nasal High Flow Therapy in the neonatal unit is an increasingly popular alternative to nasal continuous positive airway pressure (nCPAP). In neonatal units it is being used as a form of non-invasive respiratory support in its own right, and is generally considered to be a step down from ventilation, or a step up from low flow oxygen.
The modes of action of nHFT can be read in Miller (2012) or Kopuri and Ives (2014). However nHFT is fundamentally ‘the delivery of heated and humidified respiratory gas through a nasal cannula system at flow rates that exceed the patient’s demands. With a result that more efficient oxygen therapy occurs and an impact is seen on ventilation by way of dead space wash out’. Miller (2014)
In order for the respiratory support to be effective and comfortable for the patient, precise heating and humidification of the respiratory gases are required (be this air or a blend of air and oxygen). In the UK there are different devices in the market that can deliver nHFT, either as a stand-alone therapy or in combination with other forms of respiratory support or ventilation. Vapotherm, Optiflow, Fabian and certain ventilators are examples of those devices.
This guideline is intended to be a nursing guideline, providing generic guidance for neonatal nursing staff, caring for an infant being cared for on nHFT. User instructions for different high flow devices or ventilators will not be given, as user manuals and local training procedures should be covering this aspect of care. Specific discussion of a particular medical device will only be made if pertinent to improving nursing care.
5.0 Practice guidelines
5.1 Commencing nHFT
- Infants should be nursed in a safe environment. There should be access to suction, oxygen and resuscitation equipment at the bedside. These should be checked at the beginning of each shift.
- There should be access to a blood gas machine
- The nHFT machine and associated fitments should be clean and well maintained.
- The nHFT and associated circuits and cables should be used in accordance with health and safety guidelines.
- The nHFT and associated circuits/nasal prongs should be used in accordance with manufacturer’s guidelines.
- Guidance cards showing basic user instructions should be attached to the nHFT machine, and the user manual should be readily available if required.
- The nHFT stand should have brakes on it and these must be used.
- Some nHFT machines can be used with different sized cartridges, depending on the size of the machine, so care must be taken to select the correct one. For example the correct cartridge for the Vapotherm machine would usually be the low volume cartridge that allows maximum flow rates of 8 l/min. The other choice is an 8-40 L/min cartridge which is generally more suitable for an infant likely to be nursed in a paediatric ward or setting.
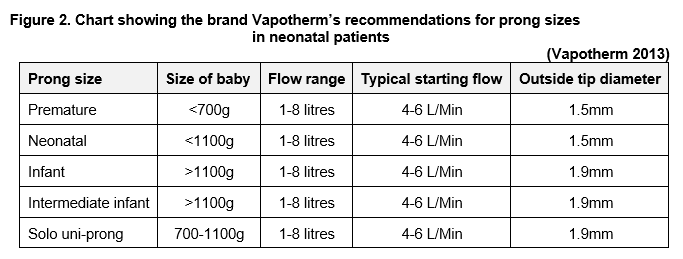
- Select the correct size of nasal prongs for the baby;
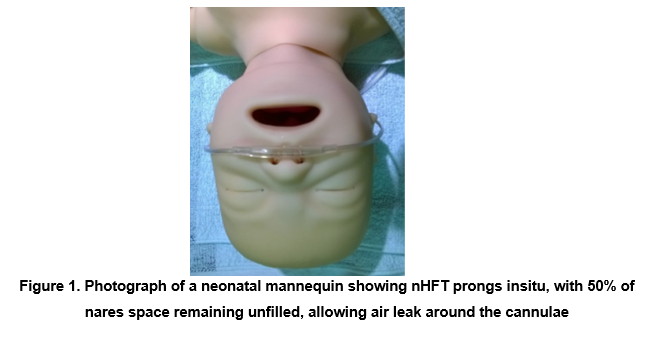
The cannulae should be loose fitting at the nares so that there is air leak around the cannulae. General recommendations are that the cannula should not take up more than 50%, and never exceed 80% of the nares, which in practice means the diameter of the cannulae should be no more than half to two thirds of the diameter of the nares. (see photograph below)
- Bi-lateral nasal prongs have been found to give the most effective respiratory support, so should be used as first preference.
- Single prong nasal prongs are available for some brands of nHFT machines. These may be useful for infants with a unilateral cleft lip and palate that prevents the siting of the bilateral prongs. In very small infants whose nostrils are too small for the smallest manufactured size of prongs, a single prong may enable one nostril to provide the necessary leak. It should be noted that the Vapotherm Solo prong has the outside tip diameter of the Infant prongs. Care should be taken to alternate nostrils with nursing shifts and to be vigilant for nasal trauma from what may be a more snug-fitting single prong. It is also essential to make sure that the other nasal passage remains patent.
- Only use nasal prongs designed for use with the machine that will be used;
- ‘Standard’ low flow nasal prongs must not be used- as the fit of the prongs in the nares required for nHFT, is different, and the long extension length of the tubing would mean respiratory gases will have cooled and humidity condensed before reaching the baby.
- Vapotherm and Fisher and Paykel cannulae are not interchangeable.
- A sterile water bag should be used when setting the machine up. A rigid container cannot collapse as it empties and would need a vented cap.
- The nHFT gas flow rate, humidification temperature and FiO2 should be set up in discussion with the medical team, and as directed by local guidelines. Commencing the gas flow rate around 4-6 L/min is common practice, with the oxygen set at the infant’s current requirement.
- Staff should be vigilant to ensure that all the components of the Vapotherm delivery cartridge and tubing have been securely connected together. More than one incident has been reported where a baby was placed onto Vapotherm and appeared to be receiving nHFT. However, when the baby became unstable it was identified that the baby had not been receiving flow from the Vapotherm, because the system was not set up correctly. Whilst the cartridge and delivery tubing were attached to each other, they were not securely or effectively connected together and the baby’s respiratory status was compromised.
- Before commencing the nHFT staff must ensure they can feel gas flow coming from the delivery tubing. This is an additional safety measure instigated following the problems outlined above.
- Place cannula onto the infant before attaching the delivery tube.
- Allow system to reach set temperature before connecting the delivery tube to the cannula.
- Continuous heart rate, respiratory rate and oxygen saturation monitoring should be in place.
- In an infant with a significant oxygen or rapidly increasing oxygen requirement or an unstable infant, the use of transcutaneous CO2 monitoring should be considered.
- The infant should have an oro-gastric tube (OGT) in situ so that the stomach can be aspirated at least 4hourly- to aid in the prevention of abdominal gaseous distention. This can be placed after commencing the nHFT- if there is an urgent need to commence the nHFT support.
- A naso-gastric tube (NGT) may be used in a larger infant, who is settled on nHFT as their nasal passage may be large enough to allow effective dead space washout and space for the NGT.
5.2 Ongoing care
- nHFT circuits should be humidified at all times. Check regularly that there is a supply of sterile water in the bag. When the bag is empty replace with a new one.
- Water vapour may condense inside nHFT tubing, this must be removed as soon as it is noticed, as it can move and blow into the infant’s nose causing distress and affecting their breathing.
- Blood gases should be taken according to clinical need, and according to local policy. Usually this would be discussed between the nursing and medical team on the ward round. A baby in air on nHFT does not need blood gases unless there is concern that they have a metabolic acidosis.
- Maintain the infant’s saturations within locally agreed settings.
5.3 Weaning nHFT
- Where available, weaning the nHFT should be according to local written weaning protocol.
- Weaning the nHFT should usually be discussed jointly between the nursing and medical teams. This will often be on a ward round.
- Whatever weaning regime, or step is decided, document actual and planned changes in the nursing care plan and nursing evaluation.
- Document how infant coped with regime.
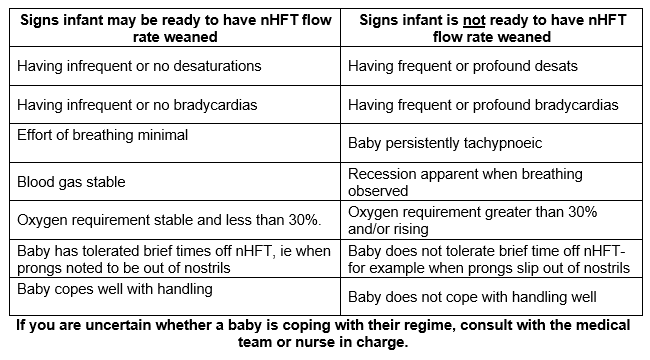
- If an infant’s nHFT setting is weaned and then the infant has a desaturation or bradycardia, this does not necessarily mean the infant has to go back up to the higher flow rate. The occasional desaturation or bradycardia may be ‘normal’ for them. See the list below for guidance.
- If an infant is being cared for using ‘Optiflow’ and requires a flow of less than 2l/min the manufacturers recommend discontinuing high flow and transitioning the baby to non-humidified low flow oxygen. The humidification is not found to be effective at flows below 2L/Min.
5.4 Positioning
- Positioning the infant prone is known to have a wide range of benefits, especially for the preterm infant with respiratory distress. However, for all infants, but especially those who require a long period on nHFT, consideration must be given to the developmental and social needs of the infant as well. A range of positions including lateral and supine are likely to be best for the infant, so each infant should be assessed individually and positioned with consideration of all their needs.
- Positioning aids can be used as appropriate to maintain comfort and correct positioning.
5.5 Tubing
- nHFT circuits are for single patient use and should be changed as per manufacturer’s guidelines and recommendation.
- Usually 30 days for Vapotherm circuits.
- Usually weekly for Optiflow circuits.
- Usually weekly for ventilator associated tubing.
5.6 Nasal prongs
- nHFT prongs are for single patient use and should be changed as per manufacturer’s guidelines. This is usually weekly, but prongs may be changed more frequently if they are coated by mucous/ nasal secretions or if there is any concern that the gas flow to the baby may be affected.
- Prongs should be positioned correctly so that they are square onto the nose and not tipped at an angle and the tips of the prongs should be well inside the nares.
- The eyes should be clearly visible without any of the prong or its securing tape touching them.
- Take extra care to ensure that the nose is not pulled upwards to minimise trauma to the base of the nasal septum,
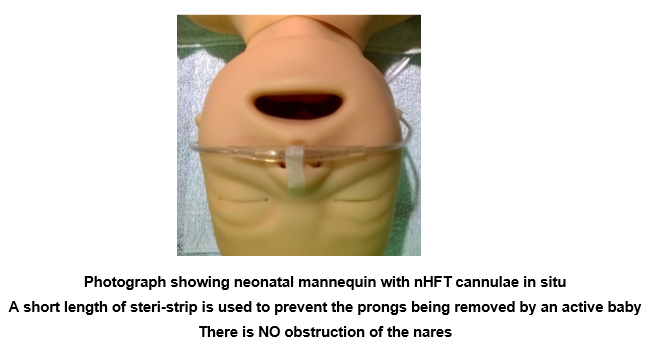
- The use of dressings is NOT recommended as a preventative measure to protect the skin. However, where an infant is repeatedly removing the nasal prongs from their nostrils, it has been found helpful to use a steri-strip running down the infant’s nose and onto the central section of the prongs. This helps to secure the prongs in place, without forcing the prongs against the nasal septum, in a way that might be uncomfortable, or damage the infant’s skin integrity. Be sure not to occlude the nostrils in any way if a steri-strip is used (see photograph below).
5.7 Flow
- Decision on gas flow rate should be made between the medical and nursing staff and documented in the care plan and notes.
- Indications for adjusting flow are:
- Degree of RDS.
- Effort of breathing.
- Oxygen requirement.
- Unsatisfactory blood gas.
- Apnoeas, bradycardias and desaturation events.
- Medical staff should be informed of any change in the infant’s condition and a blood gas should be considered.
- If there is a sudden need to increase the flow rate significantly (that is by 2 or more L/Min), then inform the medical staff and nurse in charge, as this could be indicative of a more serious problem, e.g. pneumothorax or need for intubation and ventilation.
5.8 Accessories
- If an infant requires nebulised medication, commercially made adaptors are available that enable the nHFT function to be uninterrupted, but allow ‘inline’ nebulisation. A different adapter is required for each brand of nHFT equipment.
- The adapter is not for continuous use, and should be removed after each treatment.
- Each adapter ‘kit’ is for single patient use, but can be reused if it is cleaned and dried according to manufacturer’s instructions.
- It is important to retain the proper upright orientation of the adapter during the drug administration process, so that the liquid does not spill out or fail to be nebulised.
- Some brands of nHFT can also be used with Nitric Oxide and/ or Heliox (helium-oxygen gas mixture.) Contact individual manufacturers for more details.
5.9 Humidification temperature
- Set the temperature to 37°C.
- For vapotherm, when the gas flow is running at 5L/Min or less staff have noticed increased levels of condensation (rain out) in the delivery tubing or nasal cannulas. In the circumstances where ‘rain out’ is seen, it is agreed practice to reduce the humidification temperature by 1°-3C, down to a minimum temperature of 34°C. This usually has the effect of reducing the condensation – which is at risk of spraying up the baby’s nose.
5.10 General care
- Suction may be required, this should be available and individualised to the infant’s needs.
- Ensure the prongs and connected delivery tubing are positioned in such a way that the infant’s movements are not restricted, and that the infant is not lying on any part of the tubing.
- The ogt/ ngt should be aspirated prior to every feed to empty gas and reduce the risk of abdominal distension.
- If an infant is not being fed, the ogt/ngt should be aspirated a minimum of every four hours, and more frequently if required. It is possible to leave the tube end open or with a syringe barrel attached to the end, however there is a risk that stomach contents will pass up and out of the tube.
- Ensure that the infant’s face is kept clean and free from secretions.
- If the infant’s oxygen requirement rises significantly (especially above 40%) inform the medical staff and the nurse in charge as this may be indicative of a more serious problem.
- nHFT may be an uncomfortable and possibly painful experience for infants due to the loud noise levels, and high gas flow through the mouth and nose. Staff should be vigilant for signs of pain and discomfort or distress and should seek to modify infant’s environment and offer developmental care where appropriate. For example, kangaroo care, nesting, non-nutritive sucking, containment holding or a cuddle.
- Some infants will be able to take sucking feeds whilst being supported on nHFT however studies have shown that the pressure of airflow provided by nHFT and also nCPAP alters the swallowing mechanism, and increase the risk of aspiration. Therefore, the decision to offer sucking feeds to a baby on nHFT should be made with caution, and be guided by individual assessment which includes;
- Infant feeding readiness cues and developmental maturity not gestational age.
- Physiological stability during non-nutritive sucking and tube feeds.
- The underlying reasons the infant requires respiratory support, understanding that respiratory challenges pose the biggest challenge to safe and efficient feeding.
- Medical comorbidities.
- Method of feeding – breastfed infants typically feed more safely than bottle fed infants in HFT as breastfeeding is a more responsive feeding method
As a base level, current guidance indicates that for nHFT an infant on 3L/Min and in less than 30% oxygen has a good chance of tolerating a sucking feed. Starting infants oral feeding when they require higher levels of respiratory support from nHFT does not lead to faster feeding tube weaning.
An infant post term with chronic lung disease or other chronic medical needs may be able to manage sucking feeds on higher levels of respiratory support than 3L/min and 30% oxygen, but would require specialist feeding assessment before this decision is made.
5.11 Automated Oxygen Titration through nHFT device
- Relatively new for neonatal nHFT care is the option to utilise a module attached to the nHFT device which will automatically titrate the oxygen delivered to the baby, using second to second feedback based on the infant’s oxygen saturation levels.
- Currently only available for use with Vapotherm precision flow, the Oxygen Assist Module (OAM) is an optional module intended to treat patients including neonates, in a monitored clinical environment like a neonatal unit.
- The infant has their usual oxygen saturation probe connected to their monitor. In addition, they have a second saturation probe, which connects via an extension cable to the OAM. An oxygen saturation target is set, and then the OAM will alter the oxygen delivered to the infant through the nHFT machine, in order to achieve oxygen saturation within the target range.
- The main benefits identified are;
- An increase in the proportion of time an infant’s oxygen saturation levels remain within the target saturation range.
- Potential resulting improvement in physiological stability-reduction in hypoxia and hyperoxia.
- Potential reduction in nursing workload, to respond to changing inspired oxygen requirements.
- Potential reduction in noise levels due to less alarm triggers, due to more stable oxygen saturation.
- Potential disadvantages.
- If the saturation probe is not secured correctly and gives an inaccurate oxygen saturation reading, the OAM will deliver a higher oxygen concentration than the infant actually requires.
- A baby whose respiratory status is declining may not be identified as quickly as usual by the nursing or medical team because desaturations, apnoeas or signs of increased work of breathing are masked by a gradual automated increase in the inspired oxygen requirement.
- Requires a specific pulse oximetry probe, so neonatal units may need to order in and store additional equipment specifically for the OAM device.
- Manufacturer’s instructions for use should be read before use.
- All staff should receive training before using this module.
- The main principles for safe use include;
- Always have separate and independent patient monitoring in situ.
Before use;
- Always have separate and independent patient monitoring in situ.
-
-
- Set the saturation target, and upper and lower range limits based on the agreed alarm settings of your neonatal unit.
- Set the module to neonate setting.
- Set an oxygen alarm limit, above which the OAM will alarm to tell the caregiver the limit is being exceeded.
- Set the back-up oxygen limit, at which the system will deliver oxygen, if there are any interruption to or failure of the system.
- Do not initiate automatic oxygen delivery with the Oxygen Assist Module until the patient’s SpO2 is stable.
- Every hour document;
- The oxygen saturation from the independent patient monitor.
- The oxygen saturation from the OAM
- The average oxygen administered in the previous 60 minute period- found within the trend display.
- Check that both oxygen saturation probes are correctly and securely positioned, and ensure they reading are the same or within 1-3% of each other.
-
- Problem solving.
- The OAM can be returned to ‘manual mode’- where Inspired oxygen levels are controlled by the care giver, by pressing the ‘O2 Mode’ button.
- The OAM can be overridden at any time, by turning the oxygen control dial on the main nHFT machine, the oxygen will change according to the % selected by the care giver, and will not revert to auto mode, until it is intentionally selected and started again by the care giver.
5.12 nHFT Transfer Unit
- The gas supply of oxygen and air required by a nHFT machine, is usually provided through wall ports connected to the building’s medical gas supply. Because this limits the places a NHFT machine can be used, manufacturers have now made transfer units, which allow the mobile delivery of nHFT within the hospital environment.
- These units enable the safe transfer of neonates within the hospital, to access areas such as CT scanner, operating theatre, Ultrasound departments or to visit hospitalised parents unable to visit the baby themselves. In addition, they allow warm humidified nHFT support to be made available in the delivery room, to a baby immediately after birth on the resuscitaire, or even at the mother’s side, whilst delayed cord clamping is occurring.
- The battery life will limit how far and for how long a baby can be transferred, without needing to plug the unit in again. In addition, the gas cylinders will have a time limit, dependent on the O2/air gas ratio and flow rate settings. So users will need to know the manufacturer’s guidance on this.
- See local guidelines for full user instructions, however, general principles of care include;
- Keep the machine plugged in and charging at all times when not in use, to ensure full charge is available when required.
- Replace gas cylinders when less than half empty, to maximise gas availability and hence use time, when required.
- The device can be left ready for use with a clean nHFT administration set insitu, however the humidification fluid must NOT be run through the tubing, or moisture may encourage the growth of organisms that could infect the infant when the set is eventually used.
- If a unit chooses to have the device fully ready for use, with the water run through and turned on, for example in preparation for an anticipated delivery, it may be safely stored in this way, if the manufacturers guidelines are followed. This is often requires leaving the nHFT device running, but with a minimal flow of 1L/min with the humidification turned on, which will prevent stagnation of the water and growth of organisms. Where possible, the machine should be plugged into the wall gas supply, so that the gas cylinders are not run down unnecessarily.
5.13 Parents
- Keep parents/carers informed about their infant’s progress on nHFT.
- Encourage and support parents/carers to interact with and care for their infant whilst on nHFT.
- Ensure that parents understand the steps in the weaning process and signs that the baby may need more support.
- If the infant is stable, parents/carers should be encouraged to cuddle and/or have Kangaroo care with their infant.
5.14 Documentation
- Use local nHFT care plan if available.
- One hourly observations should be performed and recorded for each infant. These include:
- heart rate
- respiratory rate
- oxygen saturations
- transcutaneous pO2 and pCO2 if in use
- flow of gas
- fiO2
- humidity temperature
- skin checks (nose/ face)
- infant’s position
- A blood pressure should be taken at least 24 hourly.
- Any agreed changes in nHFT flow or humidity temperature should be documented.
5.15 Problem solving
- If the infant has a runny nose/ wet face – not obviously caused by saliva, it is possible there is a problem with excessive condensation.
- The initial action should be to wipe the moisture from the infant’s face and nose. Also to remove any obvious build-up of moisture on the nasal prongs- by removing the prongs from the infant briefly, and flicking the prongs to remove the water.
- Consider reducing the humidification temperature setting by 1°C.
- Consider an environmental cause, such as a cold draught from an air conditioning unit blowing onto delivery tubing. Consider altering air conditioning settings, or if possible relocate machine out of the air current. If this is not possible it may be necessary to protect delivery tubing from cold draughts to prevent this problem.
- Check if using the Vapotherm machine that there is water in the full length of the delivery tubing. If a section of air has built up in the water filled compartment, this would cause the temperature to drop in that section of the tubing, and condensation to develop. The air collection can be flicked up the tubing until it returns to the main cartridge and is expelled.
- If Fisher and Paykel ventilator tubing is being used, the short section of blue inspiratory tube can be removed, so that the temperature probe is closer to the baby, this will often reduce excessive condensation.
- If an infant suddenly becomes unstable whilst nursed on nHFT (i.e. increased work of breathing, significant oxygen requirement) staff should check that there continues to be a flow of gas to the baby through the delivery tubing. This is because there have been incidents reported when the gas flow to the baby has ceased on the Vapotherm machine- but the machine has not alarmed indicating there was a fault. If there is found to be no gas flow, the infant should receive respiratory assistance such as face mask CPAP until they have recovered and the nHFT machine is replaced.
5.16 Ceasing nHFT
- When taking an infant off the nHFT, there is the possibility the infant will not manage without the respiratory support, and may require placing back onto the nHFT again. When this is a possibility some neonatal units are choosing to leave the nHFT machine next to the infant’s bedside, with the gas flow turned down but not off. There is concern that allowing the system to cool down with static air inside it will encourage the growth of organisms which could then be passed to the infant when the nHFT is placed back on the infant again. There are no clear manufacturer guideline or research findings to identity whether the humidification and gas flow should be left on. Some neonatal units have chosen to leave the nHFT system turned on and running at 1 L/Min for up to a week in case of the need for reuse on the patient.
5.17 Care of the nose and face
Every hour check visually:
- The prongs are positioned correctly.
- The nose should not be squashed or pushed upwards.
- The eyes should be clearly visible, free of both prongs and tape used to secure the prongs.
- The nasal prongs and extension tubing that continues around the back of the infant’s face should not be too tight and should certainly not cause indentation, or pitting.
At least four hourly check physically:
- The nose should be inspected for signs of redness, skin breakdown, bruising or indentation. The prongs can irritate or damage the mucosa inside the nostrils – so this should be checked too. Any alteration in appearance should be reported to the medical team and documented.
- Prongs should be checked to ensure that they are clean and patent.
- The ears should be inspected for signs of pressure damage, as the nasal prong tubing crosses the ears, and can be a source of pressure trauma, especially if the infant is laid prone with the weight of its head on its ears.
Remember:
- Regular mouth care should be performed.
- Suctioning should NOT be routine but as dictated by the infant.
- It is important that documentation is completed when the nose is checked and any changes noted.
6.0 Appendix
Useful links to videos showing how to set up nHFT systems.
(65) Vapotherm Precision Flow | In Service Video | Customer Training and Onboarding – YouTube
(65) Optiflow™ Junior 2 Introduction and Fitting Guide | F&P Healthcare – YouTube
Version Control:
| Version | Date | Details | Author(s) | Comments |
| 3 | July 2018 | Sent for ratification | KR | Lead nurses and practice educators group- approved with agreed amendments. |
| 3 | Nov 2018 | Updated by QC group | KR | Approved with amendments 01.11.2018 |
| 4 | June and Nov 2022 | Updated by QC and now Guideline group.
|
KR | To go for ratification Jan 2023 |
| Review Date: | January 2026 | |||
Document version
Version 4
Lead Authors
Thames Valley & Wessex Neonatal Network Guideline Group
Approved by
Thames Valley & Wessex Neonatal Network Governance Group
Approved on
26 January 2023
Renew date
January 2026
Full guide
Related documents and references
Canning. A et al (2021) Oral feeding for infants and children receiving nasal continuous positive airway pressure and high flow nasal cannula: a systemic review. BMC Pediatrics 2021 Feb 17;21(1):83
Chen. J et al (2020) The comparison of HHHFNC and NCPAP in extremely low birth weight preterm infants after extubation: A single center randomised controlled trial. Frontiers in Pediatrics. June 2020, Vol 8, article 250, p1-6
Dysart.K et al (2009) Research in High Flow therapy: Mechanisms of action. Respiratory medicine. Doi:10.1016/j.med.2009.04.007 p1-6.
Ferrarra. L et al. (2017) Effect of nasal continuous positive airway pressure on the pharyngeal swallow in neonates. Journal of Perinatology 37,398-403
Holme.N and Harrison.C (2012) Should we be using high flow therapy on the neonatal unit? Infant. Vol 8, No 6, pp172-76.
Kopuri.A and Ives.N.K (2014) Guidelines for the use of nasal high flow therapy (nHFT) as non- invasive support in the newborn using the Vapotherm Precision Flow. Oxford University Hospitals Trust.
Kotecha.S.J et al (2015) Safety and Efficacy of High Flow Nasal Cannula Therapy in Preterm Infants: A meta-analysis. Pediatrics, p 136, 542-53.
Liew.Z et al (2020) Physiological effects of high flow nasal cannula therapy in preterm infants. Arch Dis Child fetal neonatal Ed, Vol 105, f87-93.
Manley.B et al (2019) High-Flow Therapy for Newborn Infants in Special Care Nurseries. The New England Journal of Medicine. May 2019, pp2031-2040.
Mazmanyan.P et al (2020) Mechanisms of nasal high flow therapy in newborns. Journal of applied physiology. Feb 20, pp822-829.
Miller.T (2012) High Flow Nasal Cannula Therapy in Neonatology, Vapotherm 3100008, Vapotherm www.vtherm.com p1-8.
Miller.T (2013) Role of pressure in high flow therapy. Vapotherm. www.vtherm.com p1-10.
NHSSGGC (2019) Humidified high Flow Nasal cannulae, Clinical guideline. Found at https://www.clinicalguidelines.scot.nhs.uk/nhsggc-guidelines/nhsggc-guidelines/neonatology/humidified-high-flow-nasal-cannulae-hhfnc/#:~:text=Humidified%20High%2Dflow%20nasal%20cannulae,the%20area%20of%20nares%201
Roehr.C et al (2016) Evidence support for using heated humidified high flow nasal cannulae in neonatolgy. Clinics in Perinatology. 43 (2016)
Siva.N and Reynolds. P (2021) Stabilisation of the preterm infant in the delivery room using high flow: A five year retrospective analysis. ACTA Peaediatrica. 2021: 110: pp2065-71.
Vapotherm (2017) NICU pocket guide. Guidelines and Best practice for Nasal High Flow Cannula (HFNC) Vapotherm.com
Warnock.A et al (2020) high Flow Nasal cannula oxygen. UHL Neonatal Guideline. Found at;
Won.Y.L et al (2020) Risk factors for treatment failure of heated humidified high-low nasal cannula as an initial respiratory support in newborn infants with respiratory distress. Pediatric and Neonatology. Vol 6, p174-79.
Yoder et al (2017) Consensus approach to nasal high flow therapy in neonates. Journal of Perinatolgy, p1-5.
Zivanovic.s et al (2019) Nasal high flow therapy as primary respiratory support for preterm infants without the need for rescue with nasal continuous positive airway pressure. Neonatology. Vol 115, pp175-81.
Implications of race, equality & other diversity duties for this document
This guideline must be implemented fairly and without prejudice whether on the grounds of race, gender, sexual orientation or religion.