Palliative, End of Life and Spiritual Care Section
The information on this page is intended for health professionals reference and use only. If you are a parent or family member looking for information about treatment, please visit unit information.
Contents
1.0 Aim of Guideline
2.0 Scope of Guideline
3.0 Guideline Summary
4.0 Guideline Framework
4.1 Background Information
4.2 The need for spiritual care in a neonatal setting
4.3 Assessment
4.4 Implementing spiritual care
4.5 Best practice in spiritual care
4.6 Staff responsibility
4.7 Documentation
4.8 Resources
4.9 Ensuring ethical and professional practice
4.10 Models of care
Appendix 1
1.0 Aim of Guideline
To guide staff working across the Thames Valley and Wessex Neonatal Network, ensuring highest quality spiritual care is offered to all babies, their parents and where relevant- their extended family and friends. For accessibility, the guidelines have been collated under distinct subheadings, however, the reader is strongly advised to read the guidelines in full and to seek the advice and support of more senior or experienced colleagues in the practice setting.
2.0 Scope of Guideline
The guideline applies to all neonatal units and maternity units covered by Thames Valley & Wessex Neonatal ODN. This includes the following hospitals:

3.0 Guideline Summary
- It is imperative that spiritual care be recognised as an essential component of nursing care. Spiritual care by nurse’s should no longer be just a fundamental expectation but is also mandated by both professional and regulatory organisations.
- Staff should develop sensitivity for detecting signals on spiritual issues, as in practice, it may not be straightforward to determine when patients are experiencing spiritual distress and spiritual assessment is likely to be an ongoing process, rather than a specific event or checklist.
- First preliminary question should be asked of parents and the answer documented in a designated place. This should be asked and recorded separately for each parent- who may have very different needs and preferences. 1) Do you have a specific faith or religion, and do you have any specific needs in relation to these?
- If a parent informs a staff member of a faith/ spiritually related objection to treatment or care, this should be documented in a designated place in both the medical and nursing record. The medical team and nurse in charge should also be informed, so that the issue can be discussed further, and care planned accordingly.
- When parents express their pastoral, religious or spiritual needs and request to be referred to the chaplaincy service, this information should be recorded, and action taken.
- Where referrals are made to other services or health professionals (i.e., chaplain/ psychologist) this should always be with the parent’s explicit consent.
- Staff should ensure they know how to access the spiritual care (chaplaincy) team, both routinely and in an emergency.
- Staff should be aware of spiritual facilities within their own hospital. For example, Chapel/ multi faith rooms/ prayer rooms, so they can direct parents, their family and friends and work colleagues to access these, when required.
- Staff should take responsibility for their role in spiritual care. However, they should expect to be supported in this by their local unit. For example, through spiritual care policies, practice guidelines, readily available cultural/ religious and spiritual information, hospital chaplaincy team and hospital chapel/ prayer facilities.
4.0 Guideline Framework
4.1 Background information
Spiritual care in a health care setting is a subject that can cause uncertainty and confusion. When health care staff discuss the concept of spiritual care, they all identify that ‘it is important’. However, on further questioning they are then unclear what spiritual care means in the health care context and what spiritual care should encompass for them, in their workplace and work role. Therefore, before considering spiritual care further, it is necessary to clarify some terms for the reader.
Commonly accepted definitions include;
- Spirituality is a way of being. This may be seen as an aspect of religious belief or may not. (http://www.enhcc.eu/enhcclibrary/nolan2006-1.htm)
- For many people who are religious, spirituality refers to the soul and its protection and nurturing through life.
- ‘Spirit’ is the essence of the uniqueness of each person, their beliefs, values and experiences. ’It is most often understood as what gives us meaning and purpose and includes those aspects of life which enable us to be truly fulfilled, such as respect for their uniqueness, dignity, values, beliefs, aims cultural expression, or lifestyle choices, as well as those ways in which we interpret difficult times, pain, loss or bereavement.
- Spiritual care is the care of the spirit.
- Spiritual care is a fundamental aspect of nursing care and attending to the spiritual needs of patients may improve their health outcomes.
- ‘Religious care’ is the meeting of spiritual needs, expressed through a religious belief or commitment.
Literature identifies that in general, the physical aspects of disease management are acknowledged and considered in nursing care, but that for much of the time, spiritual care of the patient and their extended family is often not formally acknowledged as a nursing priority. This is despite growing evidence to suggest that spiritual support improves outcomes.
Authors identify factors in the clinical environment that have been found internationally to impede spiritual care delivery by nurses. These include time constrains, limited understanding, lack of recognition of its importance, lack of confidence and lack of education. The result of this deficit is noted by authors to result in the provision of spiritual care that is often poor quality and limited in its scope, with the quality of this care depending significantly upon the personal preferences and inclinations of the staff members caring for a patient on any shift.
The importance of spiritual care provision by nurses is receiving widespread acceptance internationally. A similar impetus is also noted to be present within the medical profession. So as Dunn et el (2009) write; ‘As nurses spend more time with patients than any other health care provider, it is imperative that spiritual care be recognised as an essential component of nursing care. Increasingly health care providers are expected to attend to the spiritual needs of their patients. Spiritual care by nurses is no longer just a fundamental expectation but is also a mandate by both professional and regulatory organisations.
4.2 The need for spiritual care in a neonatal setting
- Life threatening illness, in oneself or a loved one brings about contemplation of fundamental spiritual and existential questions. Like other intensive care units, the NICU, by definition, confronts families with critical illness and the possibility of actual death of an infant. Parent’s may experience severe stress and suffer spiritual distress as well. (Catlin et al, 2001)
- The birth of a child is often accompanied by elation and celebration, but when a birth results in admittance to the NICU the typical emotions of joy and celebration may be tempered with anxiety and fear. Parents with a religious and spiritual world view may find their faith and spiritual lens is an important aspect of coping with their NICU experience. (Brelsford and Doheny 2016)
- A stay in hospital can involve physical needs which may be obvious, but it can also involve emotional and spiritual needs, which may be less obvious and may come as a surprise.
- Spiritual needs should be acknowledged within neonatal care, whether these are for the babies, families, or the team itself. (Caldeira and Hall, 2012.)
- Nurses should consider spirituality as an important component of holistic care. During their professional career, they should expand their knowledge and understanding of spirituality and develop tools for assessment of spiritual needs.
- Managers have responsibility to ensure that spiritual care is carried out for babies, their families and to care for the team as spiritual leaders. (Caldeira and Hall, 2012.)
- Within the health care arena, there must be greater interest in the cultivation of the nurse’s own spirituality, as well as the creation of a hospital culture that systematically provides spiritual care throughout the entire nursing staff. Health administrators and nurse managers must support the provision of spiritual care. (Dunn et al, 2009)
4.3 Assessment
Many parents with a baby in hospital have spiritual needs and will draw upon their personal resources, as well as their family and healthcare chaplaincy serve, for spiritual support. However, nurses and other health care professionals should be able to identify and support parent’s spiritual distress as a component of providing holistic care (Timmins and Caldeira – A, 2017.)
The primary purpose of any spiritual assessment is to identify specific spiritual care needs and formulate a plan of care- where appropriate- for parents. This can be achieved using a range of methods and is especially important where spiritual distress might be anticipated. For example, in a palliative care situation, or when one or more babies is seriously ill, or in a life-threatening condition.
Informal assessment.
- When considering whether parents or families would like or benefit from spiritual support in healthcare settings, the best approach is often for nurses or other health care professionals to ask them. This demonstrates a person- centred approach to care, and means that nurses can avoid making assumptions about the patient’s spiritual needs and beliefs.
- It is important to consider that not everyone has a spiritual or religious outlook on life. For some, even the suggestion of spiritual distress or need may be considered offensive. Many societies are becoming increasingly secular, with fewer people subscribing to formal religions. There are also varying perspectives within religions, and an increase in personal and selective approaches to spirituality. A person maybe be spiritual but not religious.
- The preliminary questions should be asked of parents and the answer documented in a designated place. Each parent/s must be asked separately, as they may have different faith or religious beliefs/ practices.
Whether they have a faith or religion?
Whether they have any specific needs in relation to these? - The answer from many parents may be ‘No’, to these questions, but from the discussion around these two questions staff should ensure from the time of admission, that any clinical/ medical care does not compromise the parent’s spiritual or religious beliefs. For example.
- Objections to treatment or care
- Everyday customs
- Worship needs
- Privacy and dignity
- Customs/ procedures around significant life events. (i.e., birth) (See Appendix 1)
- Parents may express their spiritual needs by raising spiritual topics, showing a reverence for spiritual items, celebrating a spiritual season in their tradition, raising existential questions about life or the afterlife.
- Where a parent’s spiritual needs are more personal, the assessment process might be more complex and ideally based on an established therapeutic relationship between the nurse and parent.
- In practice, it may not be straightforward to determine when patients are experiencing spiritual distress and spiritual assessment is likely to be an ongoing process, rather than a specific event or checklist.
Examples of possible informal screening questions are listed below. It would not usually be appropriate to ask parents all the questions listed. Rather in the context of conversation, relationship and/ or shared caregiving for their baby, the nurse/ nursery nurse may take an opportunity to bring up the topic or enquire into a parent’s spirituality.
- How does the parent keep going day by day?
- What helps the parent get through the healthcare experience?
- How has the baby’s birth/ admission affected the parent and their family?
- Who or what provides the parent with strength and hope?
- Does the parent use prayer in their life?
- How does the parent express their spirituality?
- How would the parent describe their philosophy of life?
- What type of spiritual or religious support does the parent desire?
- What is the name of the parent’s clergy, vicar, priest, pastor, rabbi, Imam?
- What does suffering mean to the parent?
- What are the parent’s spiritual goals?
- Is there a role for the their place of worship in the their life?
- How does faith help the parent cope with their baby’s illness?
Formal assessment
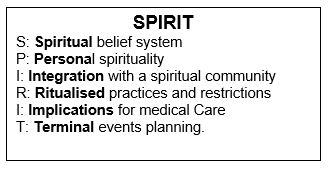
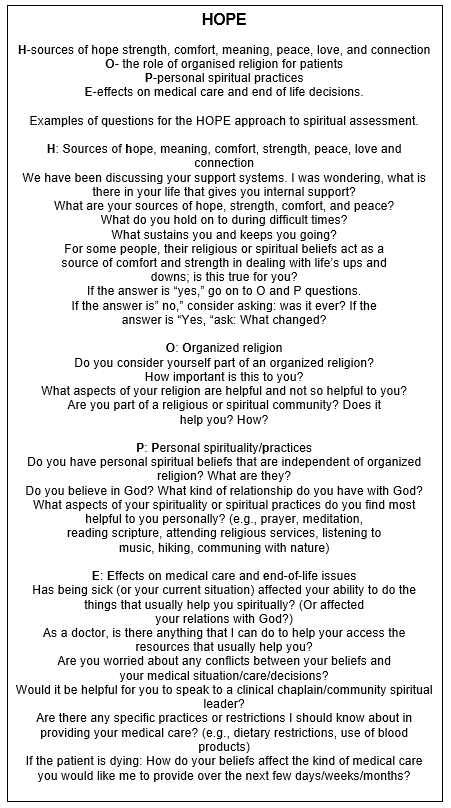
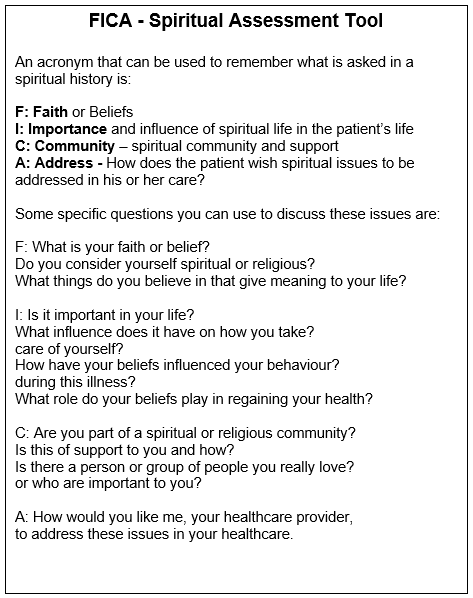
In healthcare settings most patient care plans are based on standardised assessment tools, therefore assessing and screening spiritual needs can be incorporated into a standardised assessment. Examples of three tools are shown below.
4.4 Implementing spiritual care
It is important for nurses to be aware of the different components of spiritual care. They have been described using the ABCDE acronym, seen in the table below.
Table 1. ABCDE approach. (Caldaeira and Timmins. 2017)
| Assessment | Being | Collaboration | Diagnosis | Ethics |
| Observation
Questioning Use of spiritual assessment tools |
Presence
Listening Touching Feeling |
Healthcare team
Family Other resources
|
-Identify the indicators of spiritual distress.
-Recognise the risk factors associated with spiritual distress -Evaluate the outcomes |
Be respectful
Be truthful Maintain confidentiality Provide dignity-preserving care |
Several competencies can be involved in the delivery of effective spiritual care. Up to six are identified in the recent nursing literature. These are summarised below.
Table 2. Six Core Competencies of Spiritual Nursing Care. (Caldaeira and Timmins. 2017)
| Competency | Description |
| Handling one’s own beliefs | The nurse understands their own spiritual beliefs, or lack of beliefs, and does not impose these on others. There is acceptance that beliefs vary between individuals. |
| Addressing spirituality | The nurse addresses the patient’s spirituality as an important aspect of care. |
| Collecting spiritual assessment information | The nurse asks the patient about their spiritual practices and beliefs, and the extent to which they relate to health. |
| Discussing and planning spiritual interventions | The nurse discusses spiritual interventions with the patient and their family, as well as with the healthcare team, to develop an individual care plan for the patient. |
| Providing and evaluating spiritual care | The nurse provides spiritual care and evaluates how the interventions were important in maintaining the patient’s health and well-being. |
| Integrating spirituality into institutional policy | The nurse provides care in accordance with institutional policy and has an important role in providing evidence-based care. Research emphasises that spirituality is an important dimension of care, therefore nurses should be committed to the quality and updating of institutional guidelines and policy in this area. |
If spiritual assessment identifies that a parent is experiencing spiritual distress, appropriate spiritual care interventions should be provided.
Possible spiritual care interventions for staff to consider.
- Therapeutic use of self
- Listening to parents
- Conversing with parents
- Healing presence
- Touch- where appropriate.
- Use of humour.
- Allow parent space to cry.
- Allow parent space to be silent.
- Opportunity to reminisce/ talk about deceased baby/ sibling.
- Intuitive sense- to recognise opportunity for a spiritual conversation.
- Call parents own pastor/ chaplain/ Imam
- Connect parents with local chaplain/ clergy, religious leader.
- Offer to call family members
- Offer to connect parent with other parents on neonatal unit who may have similar faith/ spirituality- and are comfortable and emotionally stable enough to connect with other parents.
- Offer to contact chaplaincy team to offer spiritual guidance regarding difficult decisions.
- A unit should ideally have an ‘Open Visiting Policy’. However, the unit visiting policy should allow flexibility for ‘visitors’ who are providing spiritual support/ care for the baby and family. For example, allowing someone else to visit the baby in their place- whilst parent takes ‘time out’. Or allowing extended periods of visiting from ‘significant others’ whether family or not.
- Give parents a spiritually nurturing environment where possible. For example, offer undisturbed time next to baby, offer privacy with screen to provide private time not ‘on view’ with the baby.
- Allow parents to have items of significance at the cot side (wrapped in plastic, as appropriate for hygiene reasons. Facilitate this through informing parents of this choice, rather than expecting them to ask for it.)
- Remember to always treat the baby with dignity, to emphasize and acknowledge the baby’s value and worth. Take care to use screens for medical procedures, maintaining confidentiality, handling baby very gently and ‘lovingly’ rather than in a ‘utilitarian’ way.
Suggestions that parents may want to consider doing.
- Read a spiritual or religious text.
- Listening to spiritual or religious recordings, chants, or songs, or speaking to baby about faith.
- Pray(er) of blessing- by parents or via chaplaincy, with others.
- Baptism of baby- via chaplaincy.
- Displaying important item at baby’s bed side (i.e.-photograph, religious image/ icon, prayer, glass angel, religion item.) These will often need to be sealed into a plastic bag for hygiene reasons
- Invite supportive friends or family member for longer visits- for support of parents for spiritual/ emotional support.
- Calling family members for support/ listening/ update.
- Prayers/ blessing/ memorial service for loved ones – perhaps if twin or siblings of multiples has died.
- Expressing creativity- perhaps to make something for the baby or for the time on the unit (i.e., knitting, making quilt, making cot card, writing blog or diary, mindfulness, adult colouring, taking daily photos, baby footprints, writing poetry- perhaps for or about the baby.)
- Taking time away from the unit. Possibly meals out, night at home.
- Time with psychologist/ counsellor/ parent listeners or Chaplain.
- Displaying family photograph/ pictures done by siblings or similar at baby’s bedside- to humanize baby’s bed space and emphasise belonging to their family.
4.5 Best practice in spiritual care
- Spiritual care should be viewed as ongoing and not just on admission. Staff should make the effort to monitor and identify different spiritual concerns as they arise in consultation with the Chaplaincy, where appropriate
- Spiritual care is inadequate if only provided when the patient requests it.
- Staff should remember that failure to address spiritual needs may add to the parent’s suffering.
- Staff should develop sensitivity for detecting signals on spiritual issues
- In an attentive conversation matter/s can be clarified for both parties
- A first step is to realise that statements made by patients/ parents/ families seldom have a singular meaning, but usually contain layers of meaning.
- Spiritual care is more likely to occur when nurses are aware of their own spirituality and personal spiritual perspectives.
- Providers should make every effort to request and record data about religion and belief.
- All parents should be asked if they wish to declare their religion or belief and have this recorded. This should be asked and recorded separately for each parent- who may have very different needs and preferences.
- When parents express their pastoral, religious or spiritual needs and request to be referred to the chaplaincy service, this information should be recorded, and action taken.
- All parents should be fully informed how their information is intended to be recorded, used and shared and of their right to consent to such processing.
- Where referrals are made to other services or health professionals (i.e., chaplain/ psychologist) this should always be with the parent’s explicit consent.
- When relevant parents should be given access to the most suitable chaplain to meet their pastoral, spiritual or religious needs.
4.6 Staff responsibility
Staff must take responsibility for their role in spiritual care. However, they should expect to be supported in this by their local unit. Access to a dedicated chaplaincy service either in house or through a local SLA.
Local units should provide.
- Spiritual care policies.
- Practice guidelines for spiritual care.
- Access to up to date religious/ cultural/ spiritual practice information- this can be via internet or e learning etc.
- Orientation for staff to existence of local hospital facilities and information on accessing the chaplaincy team, both routinely and in an emergency.
Staff should take responsibility by.
- Having an awareness of the spiritual care dimension in patient care.
- Respecting the equality and diversity agenda and Trust Policy with respect to spiritual care needs.
- Being familiar of how the spiritual care (chaplaincy) team can be accessed, both routinely and in an emergency.
- Being aware that other alternative sources of support may be accessible for parents. Modern chaplaincy services are experienced in offering a variety of religious and spiritual support and may be able to access other sources faith support, not directly represented on their teams.
- Being aware of facilities within their own hospital. For example, Chapel/ multi faith rooms/ prayer rooms.
- Being an active part of the team monitoring and identifying different parental spiritual concerns as they arise.
4.7 Documentation
- Two preliminary questions will be asked of parents (whether they have a religious denomination? and whether they practice a faith of some kind.) The answer must be documented in a designated place, so that the information can be easily accessed by all members of the health care team.
- The answers given by EACH parent must be also documented in a way that allows each parent’s response to be identified separately. Because two parents may have very different opinions and religious/ spiritual needs, which cannot be acknowledged or acted upon if the differences are not clearly identified to staff caring for a baby.
- If a parent/s informs a staff member of a faith/ spiritually related objection to treatment or care. For example, refusal to allow blood transfusions, or to receive medication with a porcine origin, this should be documented in a designated place in both the medical and nursing record, where it can be easily accessed by all the health care team. The medical team and Nurse in Charge should also be informed, so that the issue can be discussed further, and care planned accordingly.
4.8 Resources
- Parents and staff should have 24-hour access to Chaplaincy/ Spiritual Care team.
- Parents and staff should have 24-hour access to a chapel/ multi faith/ prayer room.
- There should be basic items of religious significance available on the unit for immediate access. For example.
- A copy of the Bible/ Koran and other locally significant religious texts.
- Equipment to facilitate emergency or planned baptism. Such as a copy of the words and actions required to baptise a baby, blank baptism certificates, white blanket/ white clothing for baptisms.
- White shroud for Muslim burials and preparation of the body.
- There should be temporary space identified for private parental prayer /meditation on the unit when it is not possible for a parent/ staff to access hospital communal facilities. For example, a baby is critically ill.
- Basic cultural / religious/faith information should be available on the unit for immediate access. For example, printed copies of guideline documents, or directs links to guidelines/ documents posted onto designated unit computer or hospital intranet.
- Space to enable privacy for spiritually distressed parents. This may be facilitated using screens, reallocation of a clinical space or availability of a separate ‘quiet room’.
4.9 Ensuring ethical and professional practice
- It may become apparent that the parent requires some intervention to support them with their spiritual or religious beliefs. It is important that there is no compromise between nursing staff’s personal beliefs and professional practice. So before taking any action the following should be considered:
- has the intervention been initiated by the parent?
- has clear consent been given?
- does it comply with professional codes of practice?
- does it comply with employer’s codes of practice?
- is it safe and appropriate?
- is it likely to cause offence?
- do you feel comfortable?
- do you have sufficient knowledge and skills?
- is there adequate support and supervision for you and the parent?
- When action is taken staff should ensure that there is thorough documentation in the nursing record. This should include what actions a parents may have requested, and what actions were taken by nursing staff and the outcome(s) of any intervention.
4.10 Models of care
- Spiritual care must be integrated into the nursing curriculum.
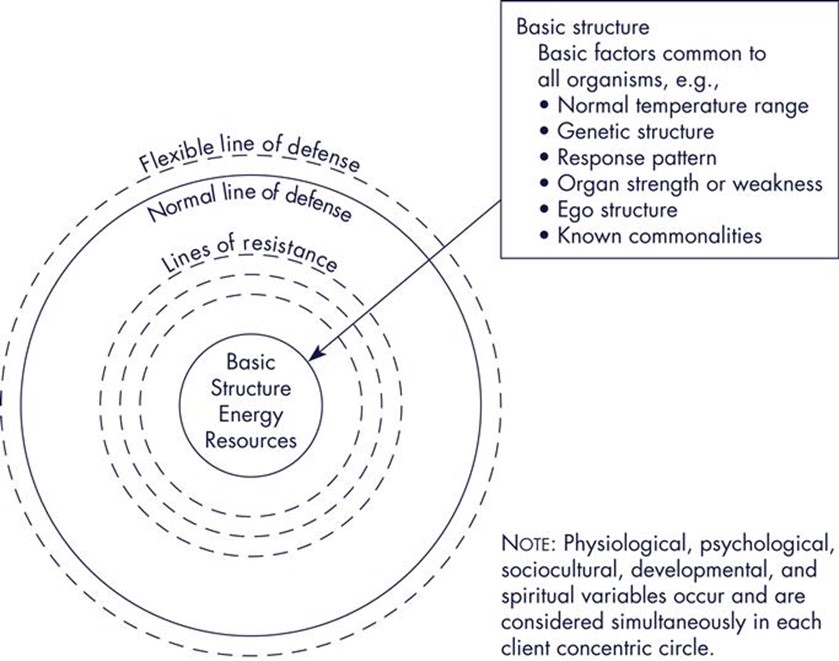
- Neuman’s Systems model is the leading nursing model to acknowledge spirituality and spiritual care. It identifies those spiritual variables are necessary for a truly holistic perspective and caring concern for the patient. It is useful for teaching spirituality to nursing students.
Neuman’s Systems Model
Appendix 1
Version control
| Version | Date | Details | Author(s) | Comments |
| Draft Version1 | December 2018 | New Guideline | Thames Valley Neonatal ODN Quality Care Group. | Reviewed by lead nurses and Practice Development Leads. |
| Draft version 1 | March 2019 | To go forward for ratification.
|
Ratified | |
| Version 3 | June 2022 | Reviewed and ready for circulation prior to ratification | Lisa Leppard | Ratified June 2022 at Governance |
| Review Date: | June 2025 | |||
Document version
Version 3
Lead Authors
- Thames Valley Neonatal ODN Quality Care Group
- Lisa Leppard, TVW Neonatal Network Lead Care Coordinator
Approved by
Thames Valley & Wessex Neonatal ODN Governance Group
Approved on
June 2022
Renew date
June 2025
Full guide
Related documents
Baldacchino.D (2016) Nursing competencies for spiritual care. Journal of Clinical Nursing, July Vol 15, No 7, pp885-96.
Brelsford.G and Doheny.K (2016) Religious and Spiritual Journeys: Brief reflections from mothers and fathers in a neonatal Intensive Care Unit (NICU) Pastoral Psychology. Feb 2016, Vol 65, Issue 1, pp79-87.
Caldeira.S and Timmins.F (2017) Implementing spiritual care intervention. Spirituality series: 3. Nursing Standard, 19th April 2017, Vol 31, No 34, pp54-60.
Catlin et al (2001) Spiritual and Religious components of patient care in the Neonatal Intensive Care Unit. Sacred Themes in Secular Settings. Journal of Perinatology, 21, pp426-30
Doe.M and Petty.S (2014) Spiritual Care Guideline, York Teaching Hospital NHS Foundation Trust, pp1-19. Found at; https://www.bing.com/search?q=spiritual%20care%20guideline%20york%20teaching%20hospital&form=SWAUA2
Dunn.L et al (2009) The provision of spiritual care by registered nurses on a Maternal –Infant Unit. Journal of Holistic Nursing. Vl 27, No 1, pp19-28.
European Network of Health Care Chaplaincy
http://www.enhcc.eu/enhcclibrary/nolan2006-1.htm)
IKN (2013) Spiritual Care Nation-wide guideline, Version1.0. Compehensive Cancer Centres (IKNL), Agora spiritual care working group. Netherlands.
Lundberg.P and Kerdonfag.P (2010) Spiritual care provided by Thai nurses in intensive care units. Journal of Clinical Nursing, Vol 19, pp1121-8
Timmins.F et (2015) Spiritual care competence for contemporary nursing practice: A quantitative exploration of the guidance provided by fundamental nursing text books. Nurse Education in practice. http://dx.doi.org/10.1016/j.nepr.2015.02.007
Timmins.F and Caldeira.S (2017) Understanding spirituality and spiritual care in nursing. Spirituality series; 1. Nursing Standard, 25th Jan 2017, Vol 31, No 22, p50-7.
Timmins.F and Caldeira.S (2017) Assessing the spiritual needs of patients. Spirituality series: 2. Nursing Standard, 15th March 2017, Vol 31, No 29, pp 47-53.
RCN (2011) Spirituality in Nursing Care: a pocket guide. Royal College of Nursing, London, March 2011, www.rcn.org.uk
Sadeghi. N et al (2016) Spiritual needs of families with bereavement and loss of an infant in the Neonatal Intensive Care Unit. A qualitative Study. Journal of Pain and Symptom management. Vol 52, No 1, July 2016, pp35-42
Yousefi.h and Abedi.H (2011) Spiritual care in Hospitalized patients. Iran Journal of Nursing and Midwifery Research, Winter 2011, Vol 16, No 1, pp125-32.
Zehtab.S and Adib-Hajbaghery. (2014) The Importance of Spiritual Care in Nursing. Nursing and Midwifery Student, Sept 2014, Vol3, No 3, e22261.
Implications of race, equality & other diversity duties for this document
This guideline must be implemented fairly and without prejudice whether on the grounds of race, gender, sexual orientation or religion.